- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Certolizumab pegol: A pegylated anti-TNF-alpha antibody fragment for the treatment of Crohn's disease
Two tumor necrosis factor-alpha (TNF-alpha) inhibitors, infliximab and adalimumab, are approved by FDA for the treatment of moderate-to-severe Crohn's disease (CD) in patients who have an inadequate response to conventional therapies. Certolizumab is a pegylated TNF-alpha inhibitor being investigated for the treatment of moderate-to-severe CD.

Key Points
Abstract
Despite the variety of medications available to treat Crohn's disease (CD), many patients' symptoms are notadequately controlled with available therapies. Two tumor necrosis factor-alpha (TNF-alpha) inhibitors, infliximab and adalimumab, are approved by FDA for the treatment of moderate-to-severe CD in patients who have an inadequate response to conventional therapies. Certolizumab is a pegylated TNF-alpha inhibitor being investigated for the treatment of moderate-to-severe CD. Because certolizumab is pegylated, it is able to be dosed less frequently than other CD therapies. In addition to a once-monthly dosing schedule, certolizumab could offer patients the conveniences of subcutaneous (SC) administration. Infliximab requires intravenous (IV) administration and a more frequent induction dosing schedule than certolizumab. Adalimumab is administered via SC injection but requires a more frequent dosing schedule during induction and maintenance compared with certolizumab. Certolizumab has been demonstrated in clinical trials to induce a clinical response and maintain remission in patients with CD; however, the agent has not been demonstrated to adequately induce remission. A BLA for certolizumab was originally filed by UCB in February 2006. FDA requested an additional phase 3 trial to assess the drug's ability to induce remission. The results of the ongoing trial, which are expected in the second half of 2008, could determine certolizumab's efficacy in inducing and maintaining remission. (Formulary. 2008;43:22–28).
Crohn's disease (CD) is an inflammatory bowel disease that affects >630,000 people in the United States.1 There is currently no cure for CD. This disease is associated with transmural inflammation of the gastrointestinal (GI) tract with systemic and extraintestinal complications. Although CD can affect any part of the GI tract, the most common areas involved are the distal small intestine and the proximal colon. Patients with CD typically develop symptoms and are subsequently diagnosed during their second and third decades of life, but people of any age can develop the disease. Common symptoms of CD include abdominal pain, fever, malaise, anorexia, and frequent diarrhea with rectal bleeding. Some patients may experience chronic symptoms, whereas others may remain symptom free for years. The course of CD is characterized by periods of remission and periods of exacerbation.1,2

Although there are a number of treatment options, many patients with CD do not achieve an adequate response to therapy, including those treated with TNF-alpha-inhibitor therapy. Surgery can be used to treat complications from CD such as abscess, fistulae, or bowel obstruction. Although not curative, surgery can also be used to control symptoms of CD when drug therapy fails.
In February 2006, UCB filed a BLA for certolizumab for the induction and maintenance of remission in patients with moderate-to-severe CD. FDA requested an additional phase 3 trial to assess the drug's ability to induce remission as the agency believed that the original studies demonstrated questionable benefit in this area. The results of the ongoing trial, which are expected in the second half of 2008, could determine certolizumab's efficacy in inducing and maintaining remission. Researchers speculated that high placebo response rates in earlier trials obscured certolizumab's efficacy in patients with low baseline C-reactive protein (CRP) levels. The ongoing trial should determine if this hypothesis is valid. The BLA addressed only the use of certolizumab in the treatment of CD; however, phase 3 trials are under way to determine certolizumab's efficacy in the treatment of rheumatoid arthritis, and phase 2 trials are being conducted to determine the agent's efficacy in the treatment of psoriasis.
CHEMISTRY AND PHARMACOLOGY
Certolizumab is the first pegylated anti-TNF-alpha monoclonal antibody. Certolizumab is a humanized antibody fragment (Fab') that is attached to polyethylene glycol to allow for less frequent administration. Certolizumab has a high affinity for human TNF-alpha, selectively targeting TNF-alpha in inflamed tissue. Although the presence of a Fab' portion allows certolizumab to retain the potency of the entire antibody, certolizumab is unable to bind phagocytic cells or to lyse cells because of a lack of an Fc portion. Antibodies typically contain a Fab' portion and an Fc portion. In these antibodies, the Fab' portion binds to the pathogen and the Fc portion binds to phagocytic cells, such as macrophages. When phagocytic cells are bound to this antibody-antigen complex, the phagocytic cells lyse the pathogen, causing death to the cell. In the case of CD, the cells that are lysed are inflamed human cells expressing TNF-alpha. The cell lysis causes adverse effects and tissue damage. 8
PHARMACOKINETICS
In dose-ranging studies, certolizumab demonstrated linear pharmacokinetics. The elimination half-life of certolizumab was demonstrated to be 311 hours. Bioavailability modeling has indicated 100% bioavailability.9 The pharmacokinetic profile of certolizumab has been demonstrated to be affected by weight. In a 70-kg patient, the volume of distribution was demonstrated to be 4.0 liters with a clearance of 0.428 L/d. Doubling of body weight was associated with a 25% decrease in maximum serum concentration (Cmax ) and a 20% decrease in the area under the curve (AUC). The presence of anticertolizumab antibodies had a >30% effect on Cmax and AUC.10 There is little available information regarding the effect of other patient characteristics on the pharmacokinetic profile of certolizumab.
CLINICAL TRIALS
Assessment tools. Researchers who conduct clinical trials involving patients with CD use a variety of assessment tools. The Crohn's Disease Activity Index (CDAI) score is the most commonly used measure in clinical studies evaluating the efficacy of therapy for CD. This score is primarily based on a patient-completed questionnaire pertaining to the severity and frequency of symptoms. Clinical response to therapy is defined by researchers as a score reduction of either ≥70 or ≥100 points from baseline; remission is defined as a total CDAI score ≤150. The Harvey-Bradshaw Index (HBI) is a simpler version of the CDAI used for data collection purposes. The HBI measures only clinical parameters including general well-being, abdominal pain, number of liquid stools per day, and abdominal mass, with higher scores indicating greater severity of symptoms; remission is generally defined as a HBI score ≤4. Because the CDAI and HBI do not address the effect of symptoms on a patient's quality of life, the Inflammatory Bowel Disease Questionnaire (IBDQ), a validated disease-specific measure, is frequently used to assess quality-of-life factors. IBDQ scores range from 32 to 224, with higher scores indicating better health-related quality of life. Remission is defined as a total score >170.
A CDAI score does not distinguish between symptoms caused by CD and those caused by other problems not related to active inflammation. The measurement of CRP, an acute phase reactant that dramatically increases during inflammatory processes, can help establish a diagnosis of CD versus other diseases in patients with symptoms of the disease/an elevated CDAI score.

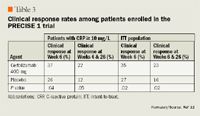
The PRECISE 1 trial was a placebo-controlled study in which patients were stratified according to CRP level (≥10 mg/L or <10 mg/L) and assigned to receive certolizumab 400 mg (n=329) or placebo (n=331) at Weeks 0, 2, and 4, and once every 4 weeks thereafter during Weeks 8 to 24 (Table 3).12 The primary end point was the percentage of patients with a clinical response (defined as a ≥100-point decrease in CDAI score at Week 6; intention-to-treat [ITT] population) and at both Weeks 6 and 26 in patients with a baseline serum CRP level ≥10 mg/L.Secondary end points were also evaluated; the first secondary end point was the achievement of remission at Week 6 (ITT population) and at both Weeks 6 and 26 in patients with a baseline serum CRP level ≥10 mg/L, and the other secondary end point was clinical response in combination with remission at Week 6 and at both Weeks 6 and 26 in patients with any CRP level. Among patients with a baseline level ≥10 mg/L, 37% demonstrated a clinical response at Week 6 compared with 26% of patients who received placebo (P=.04). Among the same group, 22% of certolizumab-treated patients and 12% of placebo-treated patients (P=.05) demonstrated a clinical response at Weeks 6 and 26. Among ITT patients, regardless of CRP levels, 35% of certolizumab-treated patients demonstrated a clinical response at Week 6 compared with 27% of patients who received placebo (P=.02). Among the same group, the response rate at both Weeks 6 and 26was 23% for patients who received certolizumab versus 16% for patients who received placebo (P=.02). The use of immunosuppressants, corticosteroids, previous treatment with infliximab, and smoking status were not demonstrated to affect the response rate. A total of 153 patients assigned to receive certolizumab withdrew from the study versus 129 patients assigned to receive placebo.
Employers Face Barriers With Adopting Biosimilars
March 1st 2022Despite the promise of savings billions of dollars in the United States, adoption of biosimilars has been slow. A roundtable discussion among employers highlighted some of the barriers, including formulary design and drug pricing and rebates.
