- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Cigna Makes Changes to Drugs Lists for 2024
Beginning Jan. 1, 2024, Cigna Healthcare’s formulary changes mostly impact generics and biosimilars.
Cigna Healthcare will remove about 150 drugs from its Standard Prescription Drug list beginning Jan. 1, 2024. (See the full list here.) Many of Cigna’s changes, with some notable exceptions, involve preferring generics over the branded therapies. Cigna would not respond to questions about these changes.
Some changes have placed generics on the exclusion list while the insurer prefers the branded products. For example, Cigna has removed from its formulary two authorized generics to treat patients with hepatitis C in favor of branded therapies. One removed generic is ledipasvir-sofosbuvir, a fixed dose combination that is a generic of Harvoni. The second is the fixed dosed combination of sofosbuvir-velpatasvir, the generic of Epclusa. The insurer has also removed the branded Mavyret (glecaprevir/pibrentasvir). Cigna is instead preferring the branded products Harvoni and Epclusa, as well as the branded Sovaldi (sofosbuvir) and Vosevi (sofosbuvir/velpatasvir/voxilaprevir), which is also approved to treat patients with hepatitis C.
Cigna has also removed the authorized generic teriparatide, which is an injection used to treat postmenopausal women with osteoporosis. Instead, Cigna favors the brands Forteo (teriparatide) and Tymlos (abaloparatide)
In addition, several drugs used for patients with cancer have been moved to nonpreferred or covered on a higher tier. For example, the cancer drug Ibrance (palbociclib) is now nonpreferred. One is Ibrance, an oral inhibitor of CDKs 4 and 6, which are key regulators of the cell cycle that trigger cellular progression. Ibrance is indicated for adults with HR+, HER2- advanced or metastatic breast cancer. Cigna prefers instead Kisqali (ribociclib) or Verzenio (ademaciclib), but the insurer has but quantity limits on both of these.
The cancer supportive therapy Ziextenzo (pegfilgrastim-bmez) also is now nonpreferred on both Cigna’s pharmacy and medical benefit. It is a biosimilar of Neulasta, which is used to help reduce the risk of infection during chemotherapy. Cigna prefers Neulasta, as well as the biosimilars Udenyca and Nyvepria.
The Humira biosimilar Amjevita was removed from Cigna’s drug list on Sept. 1, 2023. Amjevita was the first Humira biosimilars and launched in January 2023. Cigna suggests Humira and the biosimilars Cyltezo (the first FDA-approved interchangeable biosimilar), Hyrimoz-HC, and adalimumab-adaz HC (an unbranded biosimilar) as alternatives.
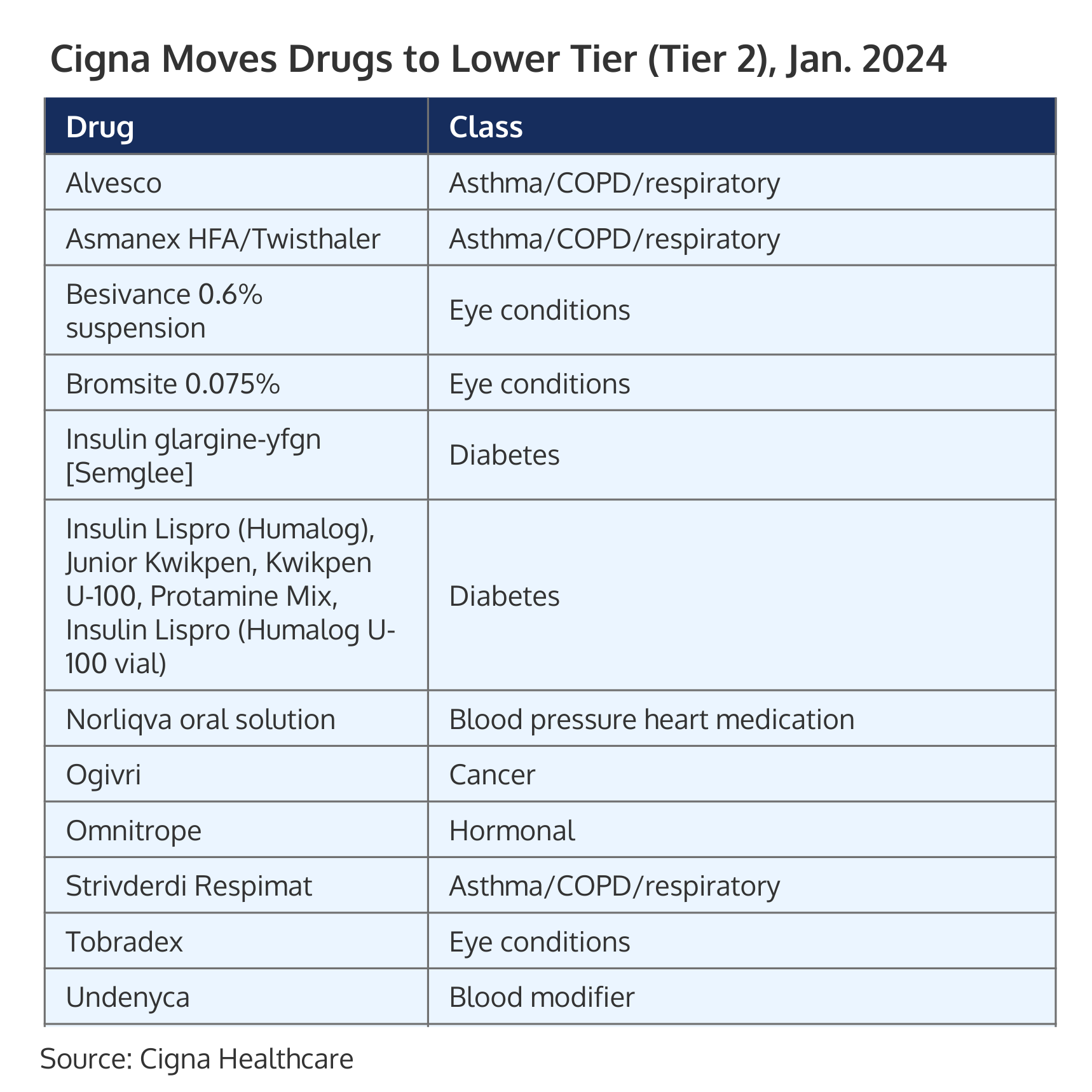
At the same time, Cigna will move several brands to a lower tier beginning in January with lower copays for patients. (See Table below.) Several insulins, including Semglee (insulin glargine-yfgn) and its unbranded interchangeable biosimilar of Lantus, as well as Humalog, will now be on a preferred brand tier (tier 2). In addition, Ogivri (trastuzumab-dkst), the first biosimilar of Herceptin, will also be preferred medication on Cigna’s medical benefit. It is approved to treat HER2+ breast and gastric cancer.
Payers Recognize the Benefits, but Still See Weight Loss Drugs through a Cost Lens
April 12th 2024Jeffrey Casberg, M.S., R.Ph., a senior vice president of clinical pharmacy at IPD Analytics LLC, a drug intelligence firm that advises payers and pharmaceutical companies, talks about how payers are thinking about weight-loss drugs.
Humira Biosimilars Have a Slow Uptake, Finds Samsung Bioepis Report
April 8th 2024Caps on Medicare Part D cost sharing as a result of the Inflation Reduction Act, could reduce members’ financial incentive for switching to a biosimilar, suggests the newest Samsung Bioepis Quarterly Biosimilar Market Report.
