- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Current and emerging treatment options for postmenopausal osteoporosis
Treatment options for osteoporosis include calcium, vitamin D, estrogen plus progesterone, calcitonin, and bisphosphonates.

Key Points
Abstract
Osteoporosis is characterized by low bone mass and microarchitectural deterioration of bony tissue, with a consequent increase in bone fragility and susceptibility to fracture. Osteoporotic fractures create a heavy economic burden, with an estimated annual cost to the healthcare system of approximately $17 billion. Currently, bisphosphonates are considered first-line therapy for the majority of patients with osteoporosis. Other current treatment options that can be used include calcium, vitamin D, estrogen plus progesterone, and calcitonin. There has been considerable progress in the development of new agents for the treatment of postmenopausal osteoporosis, including newer selective estrogen receptor modulators (SERMs), strontium ranelate, denosumab, and parathyroid hormone (1–84). Although the preliminary results from ongoing studies of these agents have been promising, further data are needed to assess the potential efficacy of these drugs for the treatment of postmenopausal osteoporosis. (Formulary. 2008;43:166–179.)

Patients with osteoporosis require safe and effective treatment options to reduce the risk of fractures. In the clinical setting, it is often a challenge to proactively provide treatment for these patients, as some patients will seek treatment only after a fracture has occurred. Postmenopausal women should therefore be considered for bone mineral density (BMD) testing, performed with dual-energy x-ray absorptiometry (DXA), for evaluation of the femoral neck, lumbar spine, and total femur every 2 to 3 years.5 A T-score of –2.5 or lower warrants a diagnosis of osteoporosis; its precursor, osteopenia, is diagnosed when the T-score ranges from –1.0 to –2.5.4,6
CURRENT TREATMENT OPTIONS FOR POSTMENOPAUSAL OSTEOPOROSIS
Calcium and vitamin D. Calcium supplementation alone provides small beneficial effects on BMD after menopause and may slightly reduce fracture rates. Calcium supplementation slows the rate of bone loss, especially in elderly women and in those with low calcium intake. A meta-analysis of 15 calcium intervention trials involving healthy women and postmenopausal women with osteoporosis demonstrated an increase of 2% in spine BMD after 2 years in patients treated with calcium supplementation versus placebo.7 The risk of vertebral and nonvertebral fracture was not reduced by a statistically significant level among women receiving calcium supplementation versus placebo. The recommended daily intake of calcium in postmenopausal women is 1,200 to 1,500 mg (through diet, supplement, or both).
Low levels of vitamin D have been associated with reduced BMD, high bone turnover, and an increased risk of falls and hip fracture among elderly individuals.7 Holick et al8 reported that 52% of 1,536 evaluated women with osteoporosis demonstrated inadequate vitamin D levels (<30 ng/mL). Studies have indicated that the daily intake of vitamin D should be approximately 400 to 800 IU.9
Estrogen and progesterone. Estrogen reduces osteoclast activity and progesterone stimulates osteoblasts, which are involved in bone formation. The addition of progesterone to estrogen therapy may help to prevent and possibly reverse osteoporosis in postmenopausal women. If progesterone plus estrogen is used for ≥10 years, the risk of fractures may be reduced by 50% to 75%.9 Treatment with conjugated estrogens 0.3 to 0.45 mg/d or estradiol 0.014 mg/d has been demonstrated to increase BMD, but the efficacy of these agents for reducing fracture incidence has not been established.11–13
Women evaluated in the WHI trial were randomly assigned to receive either conjugated equine estrogens 0.625 mg/d with or without medroxyprogesterone acetate 2.5 mg/d or placebo. The incidence of hip and clinical vertebral fractures was reduced by 33% in the estrogen plus progesterone group compared with the placebo group. After 5.2 years of follow-up, the trial was stopped because the investigators concluded that the overall health risks exceeded the benefits of estrogen plus progestin therapy. These observed risks included coronary heart disease, strokes, pulmonary embolisms, invasive breast cancer, endometrial cancer, colorectal cancer, hip fractures, and death. This trial was one of the first studies to confirm the increased risk of breast cancer resulting from the use of combination therapy with estrogen and progestin.14
A retrospective analysis of hormone replacement therapy (HRT) suggested that HRT may have a beneficial effect on cognitive function, but this effect has not been demonstrated in randomized, controlled studies.15
Selective estrogen receptor modulators (SERMs). SERMs demonstrate tissue-selective activities that produce estrogenic actions in certain organs (eg, bone, brain, and liver) during postmenopausal HRT. The 3 SERMs that are approved by FDA include tamoxifen, raloxifene, and toremifene.15,16 Although these drugs have demonstrated numerous benefits, they are also associated with very serious side effects, such as an increased risk of endometrial cancer, which limit their utility.15,17,18
Tamoxifen and toremifene are approved for the treatment of various types of breast cancer, whereas raloxifene is the only SERM currently approved by FDA for the treatment and prevention of postmenopausal osteoporosis, as well as for the reduction in risk of invasive breast cancer.17 Raloxifene slows bone thinning and causes a slight increase in bone thickness. Raloxifene also decreases resorption of bone and reduces biochemical markers of bone turnover to the premenopausal range. These effects on bone are manifested as reductions in serum and urine levels of bone turnover markers, decreases in bone resorption based on radiocalcium kinetics studies, increases in BMD, and decreases in incidence of fractures.15 Several clinical studies have demonstrated that administration of raloxifene 60 mg/d is effective in treating postmenopausal osteoporosis.17 Postmenopausal women either with or without prevalent vertebral fractures who were evaluated in the Multiple Outcomes of Raloxifene Evaluation (MORE) study demonstrated a reduction of 30% to 50% in the occurrence of incident vertebral fractures.19 The Continuing Outcomes Relevant to Evista (CORE) trial analyzed the long-term skeletal effects of raloxifene. The study reported a 30% to 40% reduction in markers of bone turnover after 1 year. Investigators observed a 2% to 3% increase in lumbar spine and femoral neck BMD after 3 years.20

In the Prevent Recurrence of Osteoporotic Fracture (PROOF) trial, the efficacy and safety of calcitonin-salmon nasal spray were compared with the efficacy and safety of placebo in 1,255 postmenopausal women.25 Patients were randomized to receive intranasal calcitonin-salmon 100, 200, or 400 IU/d or placebo for 5 years. Patients also received supplemental calcium and vitamin D. The primary efficacy end point was the reduction in risk of new vertebral fractures. Patients treated with calcitonin-salmon 100, 200, or 400 IU/d demonstrated a significant increase in lumbar spine BMD of approximately 1% to 1.5% (P<.001) compared with patients who received placebo. The risk for a new vertebral fracture was reduced by 33% in patients who received calcitonin-salmon 200 IU/d for 5 years. However, there was no significant difference among groups in the risk for nonvertebral fracture. The results of this study provided further evidence that calcitonin-salmon can improve BMD and reduce the risk for new vertebral fractures in postmenopausal women.
Bisphosphonates. Bisphosphonates are used in the treatment of postmenopausal osteoporosis because they prevent bone loss associated with estrogen deficiency, glucocorticoid treatment, and immobilization.26 These antiresorptive agents work by inhibiting osteoclast-mediated bone resorption, which leads to an indirect increase in BMD.21 There are currently 4 bisphosphonates approved for the treatment of postmenopausal osteoporosis: alendronate, risedronate, ibandronate, and zoledronic acid.27–30 Variations among these agents' pharmacokinetic profiles and chemical structures are likely responsible for the observed differences in potency.31
Alendronate is approved by FDA for the treatment and prevention of osteoporosis in postmenopausal women, the treatment of osteoporosis in men, the treatment of Paget's disease of the bone, and the treatment of glucocorticoid- induced osteoporosis in men and women with low BMD who are receiving prednisone ≥7.5 mg/d (or equivalent).27 The efficacy and safety of alendronate were demonstrated in 2 double-blind, randomized, controlled trials. Liberman et al32 evaluated 994 postmenopausal women with osteoporosis; patients were treated with either alendronate 5 or 10 mg/d for a 3-year period or 20 mg/d for 2 years followed by 5 mg/d for 1 year or placebo. Spine and hip BMD were increased by 8.8% and 5.9%, respectively, among alendronate-treated patients. The study also demonstrated a 48% reduction in the incidence of vertebral fractures among patients treated with alendronate. In the Fracture Intervention Trial (FIT), 2,027 postmenopausal women with a history of fractures were randomly assigned to treatment with either alendronate 5 mg/d (eventually increased to 10 mg/d) or placebo for 3 years.33 Compared with placebo, alendronate reduced the risk of new vertebral fractures by 47% (P<.001). Study investigators also observed a 51% reduction in hip fractures among patients treated with alendronate, but this difference was not statistically significant.
Risedronate is approved for the treatment of Paget's disease of the bone, the treatment and prevention of glucocorticoid-induced osteoporosis, the treatment and prevention of osteoporosis in postmenopausal women, and the treatment of osteoporosis in men.28,34 In the Vertebral Efficacy with Risedronate Therapy North America (VERT-NA) trial, 2,458 postmenopausal women with osteoporosis and with existing symptomatic or asymptomatic vertebral deformities were treated with risedronate 2.5 or 5 mg/d or placebo.34 After 1 year, investigators observed a 65% reduction in vertebral fractures among patients treated with risedronate (P<.001).
Ibandronate is approved for the treatment and prevention of osteoporosis in postmenopausal women. This agent was evaluated in 2 multicenter, randomized, placebo-controlled trials.35,36 The Oral Ibandronate Osteoporosis Vertebral Fracture Trial in North America and Europe (BONE) evaluated 2,496 postmenopausal women for 3 years. Patients in this study received oral ibandronate 2.5 mg/d or an intermittent dose of 20 mg every other day for 12 doses every 3 months or placebo. All study participants received calcium and vitamin D supplements during the trial. Patients treated with ibandronate demonstrated a 62% reduction in the incidence of new vertebral fractures versus a 50% reduction in the placebo group.35 The Monthly Oral Ibandronate in Ladies (MOBILE) trial randomized 1,609 postmenopausal women to receive ibandronate 2.5 mg/d, 50 mg on 2 consecutive days monthly, 100 mg monthly, or 150 mg monthly. At 2 years, the MOBILE study demonstrated an increase in lumbar spine BMD in the 4 treatment groups. Lumbar spine BMD was increased by 5.0%, 5.3%, 5.6%, and 6.6% in the daily and once-monthly groups (50+50 mg, 100 mg, and 150 mg), respectively. The study investigators concluded that once-monthly oral ibandronate is at least as effective as daily treatment.36
Zoledronic acid is a bisphosphonate derivative and an antidote for hypercalcemia. This agent is approved for the treatment of postmenopausal osteoporosis and the treatment of Paget's disease in men and women.30 Zoledronic acid inhibits both bone resorption through the actions of osteoclasts and osteoclastic activity and skeletal calcium release. Zoledronic acid also decreases levels of serum calcium and phosphorus and increases their elimination.22 The drug interactions and adverse events observed with zoledronic acid are similar to those observed with other bisphosphonate derivatives. Zoledronic acid has been associated with renal deterioration, resulting in renal failure and dialysis; this agent is not recommended for patients with severe renal impairment (creatinine clearance <35 mL/min). Patients' levels of serum creatinine, serum electrolytes, phosphate, magnesium, and hemoglobin/hematocrit should be assessed before each dose of zoledronic acid. Calcium levels should also be monitored to assess response and to avoid overtreatment.37
As a class, bisphosphonates are associated with adverse events such as abdominal pain, acid reflux, dyspepsia, nausea, and flatulence.27–30 Some of the endocrine and metabolic effects that patients may experience include hypocalcemia and hypophosphatemia.34 Treatment with alendronate, risedronate, ibandronate or zoledronic acid has been associated with bone, joint, and/or muscle pain; gastrointestinal mucosa irritation; and osteonecrosis of the jaw (ONJ). ONJ is defined as exposed bone in the maxillofacial area and occurs almost exclusively in patients receiving bisphosphonate therapy.38 Woo et al39 conducted a systematic review of 368 cases of reported bisphosphonate-induced ONJ; 65% of patients experienced necrosis of the mandible only, 26% experienced necrosis of the maxilla only, and 9% experienced necrosis of both the mandible and maxilla. Patients at risk for ONJ include patients with anemia; cancer being treated with chemotherapy, radiotherapy, or corticosteroids; infection; or pre-existing dental disease. The symptoms of ONJ include nonhealing extraction socket or an exposed jawbone. Invasive dental procedures should be avoided during treatment with bisphosphonates. Usually, the symptoms of ONJ resolve after discontinuation of bisphosphonate therapy. Bisphosphonate treatment has also been associated with esophagitis, esophageal ulcers, esophageal erosions, and esophageal stricture. Therefore, these agents should be used with caution in patients with dysphagia, esophageal disease, gastritis, duodenitis, or ulcers, as bisphosphonates may worsen those conditions.34
Teriparatide. Teriparatide is a parathyroid hormone (PTH) analog that is reserved for the treatment of osteoporosis in postmenopausal women at high risk of fracture and for the treatment of primary or hypogonadal osteoporosis in men at high risk of fracture. This agent contains the 1-34N-terminal amino acid component of recombinant human PTH and is available as an SC injection only.40 PTH stimulates osteoblast function and increases gastrointestinal calcium absorption, which increases BMD and fosters new bone formation.37
Neer et al41 randomized 1,637 postmenopausal women with a history of vertebral fractures to receive either teriparatide 20 or 40 mcg/d or placebo for 2 years. The authors reported a significant decrease in the risk of vertebral and nonvertebral fractures and increases in vertebral, femoral, and total body BMD among patients treated with teriparatide versus those treated with placebo. There was no significant difference between the 20-mcg and 40-mcg dose in the reduction of risk for fractures; however, the 40-mcg dose increased BMD significantly more than the 20-mcg dose (P<.001) and was associated with more side effects.
Although the incidence of osteosarcoma is very low in patients treated with teriparatide, the labeling for teriparatide includes a boxed warning about this condition because exposure to teriparatide has been associated with osteosarcoma in rats.40 Patients taking teriparatide may experience some central nervous system effects, such as dizziness or depression. Patients treated with teriparatide may also experience gastrointestinal adverse events (eg, nausea, dyspepsia, or vomiting), neuromuscular adverse events, skeletal adverse events (eg, arthralgia, weakness, or leg cramps), or respiratory adverse events (eg, rhinitis, pharyngitis, or dyspnea). A transient increase in calcium level has been noted 4 to 6 hours after patients are administered a dose of teriparatide.40 Patients with a history of skeletal metastases, hyperparathyroidism, or pre-existing hypercalcemia should not use teriparatide. While patients are taking teriparatide, serum calcium levels, serum phosphorus levels, uric acid levels, blood pressure, and BMD should be monitored. The transient hypercalcemia that can occur during teriparatide therapy may increase the risk of digitalis toxicity in patients being treated concomitantly with digitalis.40
INVESTIGATIONAL AGENTS
Several antiresorptive and anabolic agents for the treatment of postmenopausal osteoporosis are currently in phase 2 and 3 clinical trials in the United States. These include the SERMs ospemifene, lasofoxifene, bazedoxifene, and arzoxifene; strontium ranelate; the monoclonal antibody (mAb) denosumab; and PTH (1–84).
Ospemifene. Ospemifene is a triphenylethylene derivative that has demonstrated promise for the prevention and treatment of osteoporosis.42 This molecule was initially developed for the potential treatment of vaginal atrophy in postmenopausal women. The chemical structure of ospemifene is similar to that of tamoxifen and toremifene. Ospemifene binds to both estrogen receptors (ERs), with a slightly higher affinity for ER-alpha. In vitro studies of ospemifene in bone marrow have demonstrated its estrogen-like effects in bone through enhancement of osteoblast proliferation and differentiation. In vivo effects of ospemifene in bone have been studied in ovariectomized rat models.18,43 The effect of ospemifene 10 mg/kg on bone was demonstrated to be similar to the effects of estradiol 50 mcg/kg and raloxifene 3 mg/kg. A randomized, double-blind, phase 2 trial compared the effects of ospemifene and raloxifene on bone turnover in 118 healthy postmenopausal women.44 In this study, ospemifene 30, 60, or 90 mg or raloxifene 60 mg was administered for 3 months. Biochemical markers of bone resorption (C- and N-terminal crosslinking telopeptides of type I collagen, CTX and NTX, respectively) were evaluated through measurement of urinary output. Bone formation was also measured by assessment of procollagen type I N peptide (PINP), procollagen type I propeptide (PICP), and bone-specific alkaline phosphatase (ALP). Changes in the markers of bone formation were similar among all 4 treatment groups; however, a significant difference was observed between ospemifene 90 mg and raloxifene in PINP levels (–1.6% vs 21.3%; P<.05). These results suggested that ospemifene demonstrated beneficial effects that were comparable to or slightly better than those of raloxifene.
Lasofoxifene. Lasofoxifene is a third-generation SERM that is in phase 3 development for the prevention and treatment of postmenopausal osteoporosis.18 In December 2007, the manufacturer submitted an NDA for lasofoxifene for the treatment of osteoporosis; in September 2005, this agent was deemed not approvable for the prevention of postmenopausal osteoporosis. Lasofoxifene has demonstrated a high affinity for both ER-alpha and ER-beta. This nonsteroidal SERM has a greater potency than the other molecules in its class and is potentially a superior treatment for postmenopausal osteoporosis.45 A 2-year, randomized, double-blind, placebo-controlled and active-controlled study of 410 women with postmenopausal osteoporosis compared the effects of lasofoxifene with those of raloxifene and placebo.46 Lasofoxifene 0.25 or 1.0 mg/d significantly increased lumbar spine BMD versus raloxifene 60 mg/d (P≤.05) and versus placebo (P≤.05). Overall, the effects of lasofoxifene were greater than those observed with raloxifene.
Phase 3 clinical studies of lasofoxifene include the Osteoporosis Prevention and Lipid Lowering (OPAL) trial, the Postmenopausal Evaluation and Risk-reduction with Lasofoxifene (PEARL) trial, and the CORE (Comparison of Raloxifene and Lasofoxifene) trial.18 The OPAL study evaluated 1,907 healthy women who were randomized to receive either lasofoxifene 0.025, 0.25, or 0.5 mg/d or placebo. Increases in lumbar BMD of 1.5%, 2.3%, and 2.3% were observed among patients treated with lasofoxifene 0.025, 0.25, or 0.5 mg/d, respectively, compared with a 0.7% reduction in patients who received placebo. The PEARL trial is a double-blind, randomized, placebo-controlled study that is evaluating the prevention of fractures in women receiving lasofoxifene 0.25 or 0.5 mg/d or placebo. The CORAL trial is a 2-year, double-blind, randomized, placebo-controlled intervention trial that is comparing the efficacy of lasofoxifene 0.25 mg/d with that of raloxifene 60 mg/d.18
Bazedoxifene. Bazedoxifene is a third-generation SERM that is currently in phase 3 clinical trials for the treatment of postmenopausal osteoporosis. The manufacturer submitted NDAs for bazedoxifene for the prevention and treatment of osteoporosis in July 2007; FDA is expected to make a decision regarding approval of this drug in 2008. This SERM demonstrates agonist activity on skeletal tissue and antagonistic activity on breast and uterine tissue.18,47 Like lasofoxifene, bazedoxifene also has high affinity for both ER-alpha and ER-beta.48
Phase 3 clinical studies in progress include 3 randomized, double-blind, placebo-controlled trials.49–51 A comparison trial of bazedoxifene 20 or 40 mg versus raloxifene 60 mg or placebo is scheduled to be completed in September 2008.49 This trial will evaluate the incidence of vertebral fractures and the safety of these agents in 7,609 postmenopausal women with osteoporosis. The combination of bazedoxifene 20 mg plus conjugated estrogens 0.625 mg is being evaluated for the treatment of endometrial hyperplasia and osteoporosis in 870 women for 3 years.50 Another study is evaluating bazedoxifene versus placebo in 375 postmenopausal women.51 The primary end point in this study is lumbar spine BMD at 2 years.51 In other studies, bazedoxifene 20 to 40 mg/d has been demonstrated to reduce bone turnover by 20% to 25%.52
Arzoxifene. Arzoxifene, a benzothiophene analog, was designed to have greater bioavailability and more antiestrogenic activity than raloxifene. Because of the presence of an ether molecule in place of the carbonyl group, arzoxifene has a greater bioavailability than its parent compound (raloxifene).53 In one study, oral doses of arzoxifene 10, 20, 50, and 100 mg/d were administered to 32 patients with recurrent or metastatic breast cancer.54 At 72 hours after the first dose on Day 1 and within the 24-hour period of Day 57, pharmacokinetic sampling was performed. Arzoxifene was demonstrated to be well tolerated; 56% of patients experienced mild-to-moderate hot flashes at all dose levels.54 Two phase 3 trials assessing arzoxifene's effects on bone health were initiated in 2004.55
Strontium ranelate. Strontium ranelate is an orally active agent that consists of stable strontium and an organic moiety (ranelic acid). In vitro, strontium ranelate demonstrates anabolic and antiresorptive activity, increasing collagen and noncollagen protein synthesis, enhancing preosteoblast differentiation, inhibiting osteoclast differentiation, and reducing osteoclast function. In animal models treated with strontium ranelate, the increase in BMD has been closely correlated with increases in biomechanical bone strength.56 In a 2-year, placebo-controlled, phase 2, dose-response study involving 353 postmenopausal women with osteoporosis, treatment with strontium ranelate 2 g/d was demonstrated to reduce the incidence of vertebral fractures during the second year of treatment and to simultaneously increase BMD.57
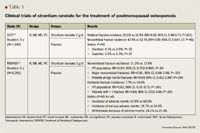
The efficacy of strontium ranelate for the treatment of osteoporosis has been assessed in 2 studies, the Spinal Osteoporosis Therapeutic Intervention (SOTI) trial and the Treatment of Peripheral Osteoporosis Study (TROPOS) (Table 1).58,59 These prospective, randomized, double-blind, placebo-controlled, phase 3 clinical trials demonstrated that strontium 2 g/d was effective and safe in reducing both vertebral and nonvertebral fractures.
In the SOTI trial, 1,649 postmenopausal women with at least 1 fracture and a low BMD (defined as <0.840 g/cm2 ) were randomized to receive either strontium ranelate 2 g/d or placebo for 3 years.58 In patients treated with strontium ranelate, the investigators noted a 49% reduction in the RR of new fractures after 1 year (P<.001) and a 41% reduction over 3 years (P<.001) versus patients who received placebo. Strontium ranelate was also associated with an increase in bone formation markers and a decrease in bone resorption markers. These changes are consistent with the theory that strontium ranelate supports bone formation and reduces bone resorption.
Using a similar study design, TROPOS evaluated the efficacy and long-term safety of strontium ranelate for the prevention of nonvertebral fractures.59 In this study, 5,091 postmenopausal women with at least 1 fracture and a low BMD (defined as <0.60 g/cm2 ) were randomized to receive either strontium ranelate 2 g/d or placebo for 3 years. In the intent-to-treat (ITT) analysis, patients treated with strontium ranelate demonstrated a 16% reduction in RR for all nonvertebral fractures (P=.04) and a 19% reduction in RR for major fragility fractures (P=.031) versus patients who received placebo. In a subgroup analysis of women at high risk for nonvertebral fractures, the RR was reduced by 36% among patients treated with strontium ranelate versus those treated with placebo (P=.046). Patients treated with strontium ranelate also demonstrated a statistically significant reduction in RR for vertebral fractures versus those treated with placebo (RR=0.61; P<.001). The investigators observed no significant differences between groups in the incidence of adverse events, the number of serious adverse events, or the number of withdrawals because of adverse events. The most common adverse events observed in SOTI and TROPOS included transient nausea, diarrhea, dermatitis, and headache.
Denosumab. Denosumab is a fully human mAb that binds to the receptor activator of nuclear factor-kappa B ligand (RANKL) with high affinity and specificity, thus inhibiting RANKL action.60 RANKL, a protein expressed by osteoblastic stromal cells, binds to the receptor activator of nuclear factor-kappa B (RANK) and serves as the primary mediator of osteoclast differentiation, activation, and survival.61
In a phase 2 study of 412 postmenopausal women with low BMD, SC denosumab 6, 14, or 30 mg administered at 3-month intervals or denosumab 14, 30, 60, or 120 mg administered at 6-month intervals increased BMD at sites rich in trabecular bone (lumbar spine) and cortical bone (femoral neck, total hip, distal third of the radius, and total body).62 The greatest response was observed with denosumab 30 mg every 3 months and 60 mg every 6 months.
Based on information derived from the biology of RANKL, preclinical models of RANKL inhibition, and phase 4 trials of bisphosphonates, some potential side effects of denosumab may include "frozen bone" (a process that leads to microfractures and brittle bone), immunosuppression, and ONJ. Although frozen bone was originally expected to occur with bisphosphonate therapy that lasted >10 years, this adverse event has not yet been observed. This adverse event may also never occur with denosumab, as this agent is completely cleared from the body.
Denosumab's potential role in the treatment of postmenopausal osteoporosis will be further defined in ongoing phase 3 clinical trials.63–65
PTH (1–84) (rDNA origin) for injection. PTH (1–84) was deemed approvable by FDA in March 2006; the agency asked for more data regarding the incidence of hypercalcemia associated with this agent and for more information about the delivery device.66
PTH is secreted by the PTH gland primarily to aid in maintaining plasma calcium homeostasis by increasing the efflux of calcium from the bone, increasing the reabsorption of calcium by the kidney, and indirectly increasing the renal synthesis of 1, 25-dihydroxyvitamin D.67,68 This hormone is catabolic with sustained exposure and anabolic with intermittent exposure.68
The Treatment of Osteoporosis with Parathyroid hormone (TOP) study examined the efficacy of PTH (1–84) in the prevention of vertebral fractures (Table 2).69 This was a randomized, double-blind, placebo-controlled, multicenter trial that randomized 2,532 postmenopausal women to treatment with daily injections of PTH (1–84) or placebo. In the ITT analysis, the incidence of at least 1 new vertebral fracture was 1.32% in the PTH group compared with 3.34% in the placebo group. At 18 months, the RR for new vertebral fractures was 0.42 in the PTH group compared with the placebo group. Patients in the PTH group also demonstrated a significant increase in spine BMD (6.9%; 95% CI, 6.37%–6.75%; P<.001) and total hip BMD (2.1%; 95% CI, 1.75%–2.47%; P<.001) versus placebo.
The hypothesis that the anabolic effects of PTH (1–84) may be enhanced when this agent is combined with a bisphosphonate was evaluated in the Parathyroid Hormone and Alendronate (PaTH) study (Table 2).70,71 To be included in the study, postmenopausal women aged 55 to 85 years were required to have T-scores <–2.5 or <–2.0 plus 1 or more of the following risk factors: aged >65 years, history of postmenopausal fracture, or maternal history of hip fracture. Criteria for exclusion included treatment with a bisphosphonate for >12 months or for >4 weeks in the previous 12 months and concurrent diseases or medications that alter bone metabolism. The primary end point of this trial was the percentage change in BMD of the lumbar spine and hip. Secondary end points included safety, adherence to treatment, and adverse events caused by study medications.
In the first phase of the PaTH study, 238 postmenopausal women were randomized to receive PTH (1–84) 100 mcg/d plus placebo (n=119), alendronate 10 mg/d plus placebo (n=60), or PTH (1–84) plus alendronate (n=59) for 12 months. Changes in the lumbar spine BMD were similar among all groups (P=not significant). However, the increase in hip BMD in the PTH (1–84) plus alendronate group was significantly higher when compared with the PTH group (1.9% vs 0.3%; P=.02) but was similar to the increase in hip BMD observed in the alendronate group (1.9% vs. 3.1%; P=.22). Bone formation and resorption were significantly increased in the PTH group (P<.001) but not in the combination group. The authors concluded that the concurrent use of PTH and alendronate should not be encouraged, as the combination may alter the distinct effects of PTH.
In the second phase of the PaTH study, the investigators examined the need for antiresorptive therapy to maintain increases in BMD after 1 year of therapy with PTH (1–84) (Table 2).71 This sequential therapy study further randomized patients into 4 different treatment groups for an additional 12 months. All patients in the PTH plus placebo group were randomized to receive either alendronate (n=60) or placebo (n=59). Patients who received combination therapy in the first phase received alendronate in the second phase (n=59), and those who received alendronate in the first phase continued to receive alendronate (n=59). Although there was a significant increase in lumbar spine BMD in all 4 treatment arms (P<.001), this increase was greatest in patients who initially received PTH and then were switched to alendronate (P<.001). Similar changes in BMD were noted for the total hip (P<.001) and femoral neck (P=.005). This trial confirmed that if antiresorptive therapy does not follow PTH therapy, most of the skeletal gains may be lost.
In both trials, there were no significant differences among groups in adherence to treatment or the occurrence of adverse events. The most common adverse events associated with PTH (1–84) in clinical trials were transient hypercalcemia, hypercalciuria, hyperuricemia, nausea, and injection-site reactions.68–70 Overall, the results of these studies demonstrated that there is no clear advantage to combining PTH with alendronate for the treatment of osteoporosis. PTH used alone followed by alendronate alone may be a preferred method of combining these 2 agents. These conclusions are in congruence with previous studies.72,73
In Europe, the PTH for Osteoporotic Women on Estrogen Replacement (POWER) study evaluated the effects of the combination of PTH and estrogen on postmenopausal osteoporosis.74 The investigators reported a significant increase in lumber spine BMD from baseline to 18 months (increase of 6.20%) and from baseline to 24 months (increase of 6.53%).
CONCLUSION
Osteoporosis is a serious public health issue that is also associated with a significant healthcare cost for society. Current treatment options for postmenopausal osteoporosis include calcium, vitamin D, estrogen plus progesterone, calcitonin, and bisphosphonates, which are currently recommended as first-line therapy for the treatment of postmenopausal osteoporosis. The risk:benefit profiles for all of these agents should be considered for individual patients. Newer agents, including SERMs, strontium ranelate, denosumab, and PTH (1–84), may eventually be additional options for postmenopausal patients who are unable to tolerate bisphosphonate therapy. Although the preliminary results from ongoing studies of these agents have been promising, further data are needed to assess the potential efficacy and safety of these drugs for the treatment of postmenopausal osteoporosis.
Dr Eaton Maxwell and Dr Maclayton are assistant professors of pharmacy practice, Texas Southern University College of Pharmacy & Health Sciences, Houston. Ms Nguyen is a doctor of pharmacy candidate, Texas Southern University College of Pharmacy & Health Sciences.
Disclosure Information: The authors report no financial disclosures as related to products discussed in this article.
Acknowledgments: The authors acknowledge Denise Darden, PharmD; Chinyere Ngene, PharmD; Jessymol Phillips, PharmD; and Uche Anadu-Ndefo, PharmD, BCPS, for their editorial assistance.
REFERENCES
1. Consensus development conference: Diagnosis, prophylaxis and treatment of osteoporosis. Am J Med. 1993;94:646–650.
2. World Health Organization. Prevention and Management of Osteoporosis: Report of a WHO Scientific Group. Geneva: World Health Organization; 2003.
3. Surgeon General's Report on Bone Health and Osteoporosis. http:// http://www.surgeongeneral.gov/library/bonehealth/docs/Chapter_4.pdf. Accessed April 30, 2008.
4. National Osteoporosis Foundation. Osteoporosis Slide Presentation. http:// http://www.nof.org/professionals/powerpointpresentation/index.htm. Accessed April 30, 2008.
5. Genant HK, Cooper C, Poor G, et al. Interim report and recommendations of the World Health Organization Task-Force for Osteoporosis. Osteoporos Int. 1999;10:259–264.
6. Raisz LG. Clinical practice. Screening for osteoporosis. N Engl J Med. 2005;353:164–171.
7. Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med. 2005;353:595–603.
8. Holick MF, Siris ES, Binkley N, et al. Prevalence of Vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab. 2005;90:3215–3224.
9. Murphy FT, Kivitz AJ, Sands EE. Management of postmenopausal osteoporosis. J Am Osteopath Assoc. 2003;103(10 suppl 6):S6–11.
10. Jackson RD, LaCroix AZ, Gass M, et al; Women's Health Initiative Investigators. Calcium plus vitamin D supplementation and the risk of fractures [erratum in N Engl J Med. 2006;354:1102]. N Engl J Med. 2006;354:669–683.
11. Estrace [package insert]. Pomona, NY: Barr Laboratories Inc; 2005.
12. Ogen [package insert]. New York, NY: Pfizer Inc; 2006.
13. Premarin [package insert]. Philadelphia, PA: Wyeth Pharmaceuticals Inc; 2008.
14. Rossouw JE, Anderson GL, Prentice RL, et al; Writing Group for the Women's Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women's Health Initiative randomized controlled trial. JAMA. 2002;288:321–333.
15. Delmas PD. Treatment of postmenopausal osteoporosis. Lancet. 2002;359:2018–2026.
16. Loose DS, Stancel GM. Estrogens and progestins. In: Brunton L, Lazo J, Parker K, eds. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 11th ed. New York, NY: McGraw-Hill Companies Inc; 2006.
17. Evista [package insert]. Indianapolis, IN: Eli Lilly and Company; 2007.
18. Gennari L, Merlotti D, Valleggi F, Martini G, Nuti R. Selective estrogen receptor modulators for postmenopausal osteoporosis: Current state of development. Drugs Aging. 2007;24:361–379.
19. Ettinger B, Black DM, Mitlak BH, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: Results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators [erratum in JAMA. 1999;282:2124]. JAMA. 1999;282:637–645.
20. Martino S, Cauley JA, Barrett-Connor E, et al; CORE Investigators. Continuing outcomes relevant to Evista: Breast cancer incidence in postmenopausal osteoporotic women in a randomized trial of raloxifene. J Natl Cancer Inst. 2004;96:1751–1761.
21. Ettinger MP. Aging bone and osteoporosis: Strategies for preventing fractures in the elderly. Arch Intern Med. 2003;163(18):2237–2246.
22. Lexi-Comp website. http:// http://www.lexi.com/. Accessed April 24, 2008.
23. Fortical [package insert]. Minneapolis, MN: Upsher-Smith Laboratories Inc; 2006.
24. Miacalcin [package insert]. East Hanover, NJ: Novartis Pharmaceuticals; 2006.
25. Chestnut CH 3rd, Silverman S, Andriano K, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: The prevent recurrence of osteoporotic fractures study. PROOF Study Group. Am J Med. 2000;109:267–276.
26. South-Paul JE. Osteoporosis: Part II. Nonpharmacologic and pharmacologic treatment. Am Fam Physician. 2001;63:1121–1128.
27. Fosamax [package insert]. Whitehouse Station, NJ: Merck & Co Inc; 2006.
28. Actonel [package insert]. Cincinnati, OH: Procter & Gamble Pharmaceuticals Inc; 2007.
29. Boniva [package insert]. Nutley, NJ: Roche Laboratories Inc; 2006.
30. Reclast [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2007.
31. Russell, RG, Croucher, PI, Rogers MJ. Bisphosphonates: Pharmacology, mechanisms of action and clinical uses. Osteoporos Int. 1999;9(suppl 2):S66–80.
32. Liberman UA, Weiss SR, Broll J, et al. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med. 1995;333:1437–1443.
33. Black DM, Cummings SR, Karpf DB, et al. Randomised trial effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541.
34. Greenspan SL, Harris ST, Bone H, et al. Bisphosphonates: Safety and efficacy in the treatment and prevention of osteoporosis. Am Fam Physician. 2000;61:2731–2736.
35. Chesnut III CH, Skag A, Christiansen C, et al; Oral Ibandronate Osteoporosis Vertebral Fracture Trial in North America and Europe (BONE). Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res. 2004;19:1241–1249.
36. Reginster JY, Adami S, Lakatos P, et al. Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study [erratum in Ann Rheum Dis. 2008;67:280]. Ann Rheum Dis. 2006;65:654–661.
37. Clinical Pharmacology [database online]. http:// http://www.clinicalpharmacologyonline.com/. Accessed April 30, 2008.
38. Watts NB, Marciani RD. Osteonecrosis of the jaw. South Med J. 2008;101:160–165.
39. Woo SB, Hellstein JW, Kalmar JR. 2006 Narrative [corrected] review: Bisphosphonates and osteonecrosis of the jaws [erratum in Ann Intern Med. 2006;145:235]. Ann Intern Med. 2006;144:753–761.
40. Forteo [package insert]. Indianapolis, IN: Eli Lilly and Company; 2007.
41. Neer M, Slovik DM, Daly M, Pott T Jr, Nussbaum SR. Treatment of postmenopausal osteoporosis with daily parathyroid hormone plus calcitriol. Osteoporos Int. 1993;3(suppl 1):204–205.
42. Gennari L. Ospemifene Hormos. Curr Opin Investig Drugs. 2004;5:448–455.
43. Komi J, Heikken J, Rutanen EM, Halonen K, Lammintausta R, Ylikorkala O. Effects of ospem- ifene, a novel SERM, on biochemical markers of bone turnover in healthy postmenopausal women. Gynecol Endocrinol. 2004;18:152–158.
44. Komi J, Lankinen KS, DeGregorio M, et al. Effects of ospemifene and raloxifene on biochemical markers of bone turnover in postmenopausal women. J Bone Miner Metab. 2006;24:314–318.
45. Terry KK, Cappon GD, Hurtt ME, Tassinari MS, Gupta U. Reproductive toxicity assessment of lasofoxifene, a selective estrogen receptor modulator (SERM) in female rats. Birth Defects Res B Dev Reprod Toxicol. 2004;71:150–160.
46. McClung MR, Siris E, Cummings S, et al. Prevention of bone loss in postmenopausal women treated with lasofoxifene compared with raloxifene. Menopause. 2006;13:377–386.
47. Stump AL, Kelley KW, Wensel TM. Bazedoxifene: A third-generation selective estrogen receptor modulator for treatment of postmenopausal osteoporosis. Ann Pharmacother. 2007;41:833–839.
48. Gruber C, Gruber D. Bazedoxifene (Wyeth). Curr Opin Investig Drugs. 2004;5:1086–1093.
49. Study evaluating bazedoxifene acetate in osteoporo- sis. clinicaltrials.gov/ website. http:// http://www.clinicaltrial.gov/ct2/show/nct00205777?term=nct00205777 &rank=1. Accessed April 30, 2008.
50. Study evaluating bazedoxifene/conjugated estro- gens combinations in healthy postmenopausal women. clinicaltrials.gov/ website. http:// http://www.clinicaltrial.gov/ct2/show/nct00464789?term=bazedoxifene&rank=4. Accessed April 30, 2008.
51. Study evaluating bazedoxifene dose-response in Japanese patients with postmenopausal osteoporosis. clinicaltrials.gov/ website. http:// http://www.clinicaltrial.gov/ct2/show/nct00238745?term=nct00238745&rank=1. Accessed April 30, 2008.
52. Ronkin S, Northington R, Baracat E, et al. Endometrial effects of bazedoxifene acetate, a novel selective estrogen receptor modulator, in postmenopausal women [erratum in Obstet Gynecol. 2005;106:869]. Obstet Gynecol. 2005;105:1397–1404.
53. Sato M, Turner CH, Wang T, Adrian MD, Rowley E, Bryant HU. LY353381.HCl: A novel raloxifene analog with improved SERM potency and efficacy in vivo. J Pharmacol Exp Ther. 1998;287:1–7.
54. Münster PN, Buzdar A, Dhingra K, et al. Phase I study of a third-generation selective estrogen receptor modulator, LY353381.HCl, in metastatic breast cancer. J Clin Oncol. 2001;19:2002–2009.
55. clinicaltrials.gov/ website. Accessed April 30, 2008.
56. Reginster JY, Sarlet N, Lejeune E, Leonori L. Strontium ranelate: A new treatment for postmenopausal osteoporosis with a dual mode of action. Curr Osteoporos Rep. 2005;3:30–34.
57. Meunier PJ, Slosman DO, Delmas PD, et al. Strontium ranelate: Dose-dependent effects in established postmenopausal vertebral osteoporosis-a 2-year randomized placebo controlled trial. J Clin Endocrinol Metab. 2002;87:2060–2066.
58. Meunier PJ, Roux C, Seeman E, et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med. 2004;350:459–468.
59. Reginster JY, Seeman E, De Vernejoul MC, et al. Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab. 2005;90:2816–2822.
60. Weiner LM. Fully human therapeutic antibodies. J Immunother. 2006;29:1–9.
61. Hsu H, Lacey DL, Dunstan CR, et al. Tumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligand. Proc Natl Acad Sci U S A. 1999;96:3540–3545.
62. McClung MR, Lewiecki EM, Cohen SB, et al; AMG 162 Bone Loss Study Group. Denosumab in postmenopausal women with low bone mineral density. N Engl J Med. 2006;354:821–831.
63. Extension study to evaluate the long term safety and efficacy of denosumab in the treatment of osteoporosis. clinicaltrials.gov/ website. http:// http://www.clinicaltrials.gov/ct/show/nct00523341?order=1. Accessed April 30, 2008.
64. A multi-center, randomized, open-label study to assess the immunogenicity and safety of denosumab in pre-filled syringe compared to vial in subjects with low bone mineral density. clinicaltrials.gov/ website. http://clinicaltrials.gov/ct/show/nct00515463?order=2/. Accessed April 30, 2008.
65. A randomized, double-blind study to compare the efficacy of treatment with denosumab versus alendronate sodium in postmenopausal women with low bone mineral density. clinicaltrials.gov/ website. http://clinicaltrials.gov/ct/show/nct00330460?order=4/. Accessed April 30, 2008.
66. NPS receives approvable letter for Preos NDA [press release]. Salt Lake City, UT: NPS Pharmaceuticals; March 10, 2006.
67. Lindsay R, Nieves J, Formica C, et al. Randomized controlled study of effect of parathyroid hormone on vertebral bone mass and fracture incidence among postmenopausal women on estrogen with osteoporosis. Lancet. 1997;350:550–555.
68. Hodsman AB, Hanley DA, Ettinger MP, et al. Efficacy and safety of human parathyroid hormone (1-84) in increasing bone mineral density in postmenopausal osteoporosis. J Clin Endocrinol Metab. 2003;88:5212–5220.
69. Greenspan SL, Bone HG, Ettinger MP, et al; Treatment of Osteoporosis with Parathyroid Hormone Study Group. Effect of recombinant human parathyroid hormone (1-84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: A randomized trial. Ann Intern Med. 2007;146:326–339.
70. Black DM, Greenspan SL, Ensrud KE, et al; PaTH Study Investigators. The effects of parathyroid hormone and alendronate alone or in combination in postmenopausal osteoporosis. N Engl J Med. 2003;349:1207–1215.
71. Black DM, Bilezikian JP, Ensrud KE, et al; PaTH Study Investigators. One year of alendronate after one year of parathyroid hormone (1-84) for osteoporosis. N Engl J Med. 2005;353:555–565.
72. Kurland ES, Heller SL, Diamond B, McMahon DJ, Cosman F, Bilezikian JP. The importance of bisphosphonate therapy in maintaining bone mass in men after therapy with teriparatide [human parathyroid hormone (1-34)]. Osteoporos Int. 2004;15:992–997.
73. Rittmaster RS, Bolognese M, Ettinger MP, et al. Enhancement of bone mass in osteoporotic women with parathyroid hormone followed by alendronate. J Clin Endocrinol Metab. 2000;85:2129–2134.
74. Fogelman I, Christiansen C, Spector T, Fraser WD, Fordham J. Safety and efficacy of PTH (1–84) at 18 and 24 months in women with postmenopausal osteoporosis receiving hormone therapy: results from the POWER study [abstract]. Presented at: 27th Annual Meeting of the American Society for Bone and Mineral Research; September 22–27, 2005; Nashville, TN. Abstract 1080.
