- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Eltrombopag: A TPO receptor agonist for the treatment of chronic idiopathic thrombocytopenic purpura
Eltrombopag is a TPO receptor agonist that is currently pending FDA approval for the treatment of ITP. This agent has been granted orphan drug and priority review status. In May 2008, the Oncology Drugs Advisory Committee unanimously agreed that eltrombopag demonstrates a favorable risk:benefit profile for the short-term treatment of chronic ITP.

Key Points
Abstract
Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disorder that can become a chronic refractory problem in adult patients who develop this disease. To date, therapies have targeted immunosuppression and inhibition of platelet destruction. Eltrombopag is a thrombopoietin (TPO) receptor agonist that is currently pending FDA approval for the treatment of ITP. Studies of eltrombopag have demonstrated that the agent is effective in increasing platelet counts in patients with refractory ITP; this increase in platelet counts is generally observed within 1 week of treatment initiation. In clinical studies, eltrombopag has been well tolerated, with headache reported as the most common adverse event. If approved, eltrombopag will compete with romiplostim, another TPO receptor agonist that was approved by FDA in August 2008 for the treatment of ITP. (Formulary. 2008;43:356–365.)
In each issue, the "Focus on" feature reviews a newly approved or investigational drug of interest to pharmacy and therapeutics committee members. The column is coordinated by Robert A. Quercia, MS, RPh, clinical manager and director of Drug Information, Department of Pharmacy Services, Hartford Hospital, Hartford, Conn, and adjunct associate professor, University of Connecticut School of Pharmacy, Storrs, Conn; and by Craig I. Coleman, PharmD, assistant professor of pharmacy practice, University of Connecticut School of Pharmacy, and director, Pharmacoeconomics and Outcomes Studies Group, Hartford Hospital.
Idiopathic immune thrombocytopenic purpura (ITP) is a relatively uncommon autoimmune disease state in the general population; the annual incidence of ITP in adults is cited as 1.6 to 2.3 cases per 100,000 per year.1 The autoimmune nature of ITP was first recognized in 1950 when the serum of a patient with ITP was administered to a physician, which led to a transient decrease in the physician's platelet count.2 ITP can occur in both adults and children. In adults, the disease process tends to be a chronic problem, with episodes of remission and recurrence. In children, however, the disease tends to be a self-limited process that typically resolves completely. Thrombocytopenia can be recognized by platelet counts <150,000 platelets/mm3; however, in patients with ITP, platelet counts <50,000 platelets/mm3 are typical.3 Patients with platelet counts <30,000 platelets/mm3 have a significantly increased risk of bleeding.
Patients with ITP may exhibit no symptoms, and the disease may be diagnosed only through routine blood work; alternatively, patients may present with bleeding, bruising, petechiae, and/or serious bleeding with low platelet counts.1 The risk of bleeding, both major and minor, is the key outcome of this disorder, as bleeding can lead to morbidity and mortality in patients with ITP or with thrombocytopenia in general.
The pathophysiology of ITP involves an autoantibody that can target and bind to platelets, leading to platelet destruction through the reticuloendothelial system. The destruction of platelets in the reticuloendothelial system, particularly in the spleen, is the rationale behind the use of splenectomy in patients whose disease has relapsed or become refractory to initial therapy. Patients with ITP may also have autoantibodies that can target the megakaryocyte, leading to decreased platelet production. Recent evidence suggests that this pathway may contribute to the disease more than had been thought previously.1,2 The causative factor leading to the loss of self-tolerance in a particular patient or in patients with ITP in general has not been identified. Studies have demonstrated that autoantibodies typically target GP IIb/IIIa or Ib/IX as antigens. Studies have also demonstrated some evidence that antibodies targeting GP Ib/IX may inhibit the megakaryocyte in the bone marrow, leading to decreased production of platelets.1,2 Involvement of T lymphocytes, particularly CD4+ T cells and autoantibody-producing plasma cells, has also been demonstrated in the ITP disease process. In addition, platelet-reactive T cells have been identified in the blood of patients with ITP.1,2
In patients with ITP, the traditional approach to treatment has been to initiate oral corticosteroid therapy, typically with prednisone 1 to 2 mg/kg/d, to increase platelet count. Generally, patients are considered for therapy with oral corticosteroids if platelet counts are <30,000 to 50,000/mm3, because of the increased risk of bleeding in these patients. Oral corticosteroid therapy increases platelet counts in approximately two-thirds of patients initially, but long-term remission is rare, occurring in approximately 10% to 15% of patients.3
When the patient has severely low platelet counts (ie, <30,000–50,000/mm3) and/or major bleeding, the use of intravenous immunoglobulins (IVIg) is warranted. One study of 122 adult patients with platelet counts ≤20,000/mm3 demonstrated that treatment with IVIg led to platelet counts >50,000/mm3 in 79% of patients at Day 5.4 A response to IVIg alone generally occurs within a few days to a week after treatment, but this response is usually transient. Patients with ITP may also be treated with IV anti-D Ig. In one study that evaluated single-dose IV anti-D Ig in 27 adults with ITP and platelet counts ≤30,000/mm3, researchers observed that an anti-D dose of 75 mcg/kg/d increased platelet counts as early as 1 day after treatment.5 Responses to anti-D Ig are rapid and persist over several weeks following therapy.
In cases of life-threatening bleeding, combination therapy with IVIg, IV methylprednisolone, and platelet transfusions is usually administered to stabilize patients and to avoid morbidity and mortality.1
Often, splenectomy will be performed early in patients who do not remain in remission with corticosteroids alone or in patients who cannot taper off corticosteroids without a decrease in platelet counts. In a review of 2,623 patients with ITP, 66% of patients who underwent splenectomy demonstrated a complete response (defined as achieving and maintaining a platelet count >150,000/mm3 or ≥100,000/mm3 for 30 days).6 A long-term complication of splenectomy is the risk for encapsulated organism infections; to counter this risk, patients typically receive vaccinations before surgery and are monitored for infections afterward.
In approximately 30% of adult patients with ITP, the disease will relapse after multiple therapies. The disease may also relapse after splenectomy. When the disease becomes refractory or relapsed after initial therapies, a variety of medications may be used to attempt to increase platelet counts. Patients may be treated repeatedly with corticosteroids; treatment with agents such as azathioprine, vinca alkaloids, cyclosporine, danazol, dapsone, mycophenolate, or rituximab may follow. Rituximab has been studied recently for patients with refractory ITP with or without splenectomy, and overall response rates of 44% have been observed, with an average duration of response of 10.5 months.7 Early use of rituximab may be able to delay the need for splenectomy in some patients earlier in the course of ITP therapy.
Eltrombopag (Promacta, GlaxoSmithKline/Ligand) is an investigational thrombopoietin (TPO) receptor agonist that is pending FDA approval for the short-term treatment of chronic ITP. This agent has been granted orphan drug and priority review status. In May 2008, the Oncology Drugs Advisory Committee (ODAC) unanimously agreed that eltrombopag demonstrates a favorable risk:benefit profile for the short-term treatment of chronic ITP.
Romiplostim, another TPO receptor agonist, was approved by FDA in August 2008 for the treatment of chronic ITP in patients who have had an inadequate response to corticosteroids, IVIg, or splenectomy. This agent is delivered via subcutaneous (SC) injection.8,9 Romiplostim will be available to registered physicians through a restricted distribution program; as part of this program, each dose of medication is to be accompanied by a patient medication guide.8
A study comparing the efficacy of romiplostim versus that of eltrombopag has not yet been conducted. In general, romiplostim therapy is most effective while the patient continues on the medication, and the agent's effects typically dissipate within a few weeks after discontinuation, similar to eltrombopag. Both agents have only limited data regarding long-term continuous management for this chronic problem.
CHEMISTRY AND PHARMACOLOGY
The TPO receptor is the target of eltrombopag. TPO receptors are located on hematopoietic stem cells, megakaryocytic progenitor cells, and platelets.10 Eltrombopag ([1,1'-biphenyl]-3-carboxylic acid, 3'-[(2Z)-[1-(3,4-dimethylphenyl)-1,5-dihydro-3-methyl-5-oxo-4H-pyrazol-4-ylidene]hydrazino]-2'-hydroxy-, compound with 2-aminoethanol) is a nonpeptide TPO mimetic hydrazone small molecule that targets the extracellular domain of the TPO receptor. The compound has 1 acidic end, 1 lipophilic end, and a metal chelate group in the center.1,10,11 It is important to note that TPO nonpeptide mimetics are species specific, activate the TPO receptor in a different way than endogenous TPO, and have additive effects with endogenous TPO.10,11
TPO is normally produced in the liver and is secreted directly into the circulation. Activation of the TPO receptor by eltrombopag triggers intracellular signaling, which leads to proliferation and differentiation of megakaryocytes. Stimulation of the TPO receptor may be caused by eltrombopag-induced dimerization of the receptor and subsequent intracellular signaling, or eltrombopag may directly activate the signal transduction mechanism.10 TPO receptor stimulation leads to activation of the JAK2 and STAT5 pathways, ultimately stimulating the differentiation of megakaryocytes from earlier progenitor cells and leading to increased platelet production and release into the peripheral circulation.10–12 During downstream signaling, intracellular MAPK activation occurs, promoting proliferation and inhibiting apoptosis.10–12 Eltrombopag increases the capacity for platelet production in the bone marrow by stimulating megakaryocytic colony-forming cells (Meg-CFCs) and early megakaryocytic progenitors, leading to increased numbers of mature megakaryocytes and increased platelet production. A study of the in vivo effects of eltrombopag on platelet function demonstrated that eltrombopag therapy does not affect or enhance platelet activation.13
A relatively new technique to determine the effect of increased platelet production versus decreased platelet destruction is the immature platelet fraction (IPF) test. Patients with increased platelet production would demonstrate higher numbers on this test, whereas patients with decreased platelet destruction would demonstrate lower numbers.14 Psaila et al14 reported IPF test results of 0.2 to 32.8, 3 to 5.6, 7.8, and 23.5 to 59 in patients treated with IVIg, anti-D, rituximab, or eltrombopag, respectively. Although these data are limited by the very small number of patients in this study, the results do indicate that eltrombopag plays a role in increasing the number of immature or young platelets during therapy.
PHARMACOKINETICS
The time to maximum concentration (Tmax) of eltrombopag is 2 to 6 hours, with a half-life (t1/2) of 21 to 32 hours. The pharmacokinetic profile of this agent is linear for doses up to 200 mg, with proportional increases in the area under the curve (AUC) in doses ranging from 50 to 200 mg. Eltrombopag is orally bioavailable.3
In a pharmacokinetic dose-ranging study, eltrombopag demonstrated dose-dependent and linear pharmacokinetics in 73 healthy adult male volunteers (mean age, 27.5 y; mean baseline platelet count, 239,000/mm3).12 Volunteers were administered eltrombopag 5, 10, 20, 30, 50, or 75 mg/d or placebo for 10 days. In the 75-mg/d cohort, the maximum concentration (Cmax) was 7.3 mcg/mL, with a corresponding Tmax of 2.5 to 5 hours, and the mean AUC was 79.0 mcg·h/mL. The mean t1/2 was >12 hours for all doses except the 5-mg/d dose, which demonstrated a t1/2 of 9 hours. With multiple daily dosing, an accumulation of 40% to 50% was noted with doses ≥20 mg/day.
Plasma eltrombopag AUC(0–tau) has been observed to be 70% to 80% higher in healthy volunteers of East Asian descent compared with non-Asian volunteers.3 Further studies in this population are warranted. The ongoing study TRA108109 is assessing Japanese patients treated with eltrombopag 12.5 or 25 mg/day.3
CLINICAL TRIALS
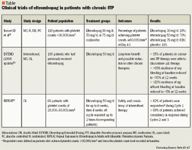
The largest trial of eltrombopag to date included 118 patients with chronic ITP.15,18 Study patients had a ≥6-month history of ITP and documented platelet counts <30,000/mm3 at enrollment, had previously been treated with ≥1 therapy for ITP, and were aged ≥18 years. Patients were permitted to continue maintenance immunosuppressive therapy if the dose had been stable for ≥1 month, but no other acute therapy was permitted within 2 weeks of enrollment. Patients were excluded if they had HIV infection, hepatitis C virus (HCV) infection, systemic lupus erythematosus, anemia with a hemoglobin level <10 g/dL, congestive heart failure, thrombosis within 1 year of enrollment, or acute myocardial infarction within 3 months of enrollment. The study was a multicenter (44 sites), double-blind, randomized, placebo-controlled trial that assigned patients to receive eltrombopag 30 mg/d (n=30), eltrombopag 50 mg/d (n=30), eltrombopag 75 mg/d (n=28), or placebo (n=29) for up to 6 weeks. Patient stratification was based on platelet counts (≤15,000/mm3 or >15,000/mm3), splenectomy, and concurrent ITP therapy. The primary end point of the study was the percentage of patients who reached a platelet count of ≥50,000/mm3 by Day 43. If platelet counts exceeded 200,000/mm3, treatment was discontinued. Bleeding was assessed using the World Health Organization (WHO) bleeding scale: grade 0, no bleeding; grade 1, petechiae; grade 2, mild blood loss; grade 3, gross blood loss; and grade 4, debilitating blood loss. The study was designed to enroll 272 patients, with interim analyses planned for when one-third and two-thirds of study accrual targets were met.
At baseline, the groups were relatively similar with regard to sex, stratification variables, and the number of previous therapies used; however, the distribution of age was uneven (median age: eltrombopag 30 mg/d, 51 y; eltrombopag 50 mg/d, 45 y; eltrombopag 75 mg/d, 55 y; placebo, 42 y; P=.04 across all treatment groups). The proportion of Caucasian patients varied among the placebo group (86%) and the groups treated with eltrombopag 30 mg/d (83%), eltrombopag 50 mg/d (60%), or eltrombopag 75 mg/d (89%) (P=.02 for whites vs nonwhites). The patients in this study were heavily pretreated; 97% of patients had ≥1 prior therapy, 74% had ≥2 prior therapies, 51% had ≥3 prior therapies, and 36% had ≥4 prior therapies. Additionally, 47% of all patients had undergone splenectomy, 32% were taking concurrent ITP medication, and 48% had platelet counts ≤15,000/mm3.
The proportion of patients achieving the primary end point (using the last observation carried forward [LOCF] method) was 28% in the eltrombopag 30-mg/d group, 70% in the eltrombopag 50-mg/d group, 81% in the eltrombopag 75-mg/d group, and 11% in the placebo group. These results were statistically significant (P<.001) for the eltrombopag 50- and 75-mg/d groups versus placebo. Similar results were noted when the data were evaluated without the LOCF method. By Day 8 of the study, 44% of patients treated with eltrombopag 50 mg/d and 62% of patients treated with eltrombopag 75 mg/d had achieved platelet counts ≥50,000/mm3; by Day 15, 88% of patients treated with eltrombopag 50 mg/d and 81% of those treated with eltrombopag 75 mg/d had achieved this goal. Based on data from the 109 patients evaluated for efficacy who completed the 6-week treatment phase, platelet counts increased to >200,000/mm3 in 14% of patients treated with eltrombopag 30 mg/d, 37% of patients treated with eltrombopag 50 mg/d, 50% of patients treated with eltrombopag 75 mg/d, and 4% of patients treated with placebo. In these patients, the platelet counts returned to near-baseline levels within 2 weeks of treatment discontinuation. Splenectomy, age, and race had no effect on efficacy. Responses were higher among those patients taking concurrent therapy who received eltrombopag 30 or 50 mg/d versus those patients who were not taking concurrent therapy.
Investigators observed that among patients treated with eltrombopag 50 or 75 mg/d, the incidence of bleeding decreased during therapy and returned to baseline during the 6-week follow-up after therapy was discontinued. The incidence of bleeding (all grades) during the study was 17% among patients treated with eltrombopag 30 mg/d, 7% among those treated with eltrombopag 50 mg/d, 4% among those treated with eltrombopag 75 mg/d, and 14% among patients who received placebo. Median baseline TPO concentrations at baseline and at Day 43 were similar for all groups and within the normal range for healthy volunteers. Quality-of-life measurements with the Short Form 36 (SF36) Version 2 health survey were relatively unchanged throughout the study.
The Eltrombopag Extended Dosing (EXTEND) study was an open-label extension study designed to assess the long-term safety and efficacy of eltrombopag.19 Patients previously enrolled in an eltrombopag study were eligible to enter this trial after a 4-week washout period. Eltrombopag was initiated at a dose of 50 mg/d and could be titrated up to 75 mg/d after 3 weeks with the goal of reaching a platelet count of ≥50,000/mm3. Once that goal was reached, other ITP medications were tapered or discontinued while platelet counts of ≥50,000/mm3 were maintained. Eltrombopag was then titrated to a minimum maintenance dose of 25 to 75 mg/d to achieve the target platelet range of 50,000 to 200,000/mm3. Data on 96 patients were reported as of August 6, 2007, with median treatment duration of 151 days. A total of 61 patients entered the study with platelet counts <30,000/mm3; 73% of these patients achieved the study goal. Ten of the 61 patients had a platelet count ≥400,000/mm3 at 1 point during the study. At baseline, 63% of patients had WHO grade 1 to 4 bleeding. The proportion of patients with WHO grade 2 to 4 bleeding was 27% during initial dose titration, 24% during tapering of other ITP medications, 7% during eltrombopag maintenance dose titration, and 4% during long-term use after titration. Comparison of these percentages is difficult, as baseline bleeding was reported as grade 1 to 4 and bleeding during the study was reported as grade 2 to 4.
Updated results from the EXTEND study were presented at the 13th Congress of the European Hematology Association.16 The study authors reported that of the 109 patients who received eltrombopag in this study, 37% were receiving other therapies for ITP at baseline, 44% had undergone a splenectomy, and 70% had baseline platelet counts <30,000/mm3. During the study, 14 patients (35%) who were taking other therapies for ITP, including prednisone and danazol, were able to discontinue those therapies. Bleeding rates decreased from >60% at baseline to <30% at 12 weeks, and significant bleeding decreased from >20% at baseline to <5% at 12 weeks.
The Repeat Exposure to Eltrombopag in Adults with Idiopathic Thrombocytopenic Purpura (REPEAT) study was also presented at the European Hematology Association meeting.17 This trial was an open-label, phase 2 study that examined the safety and continued response of repeated intermittent dosing of eltrombopag in patients with chronic ITP. Sixty-six patients with baseline platelet counts of 20,000 to 50,000/mm3 received eltrombopag 50 mg/d over 3 cycles of therapy. Each cycle consisted of up to 6 weeks on therapy with a 4-week off-therapy follow-up period. Responders were defined as patients whose platelet counts increased to >50,000/mm3 and at least twice their baseline platelet count during Cycle 1. These patients were allowed to continue on to further cycles of treatment. The median age of patients was 51 years; at baseline, 44% of patients had platelet counts of 20,000 to 30,000/mm3 and 45% had platelet counts of 30,000 to 50,000/mm3. At baseline, 33% of patients were taking other ITP therapy. Responses were noted in 82% of patients during Cycle 1. The time to response was rapid, with >60% of patients responding by Day 8 and >75% responding by Day 15. During the off period, platelet counts typically returned to baseline after 2 weeks off therapy. Investigators noted that 88% of patients had consistent responses between Cycles 1 and Cycles 2 and 3.
There are several studies currently ongoing to assess the efficacy of eltrombopag for up to 6 months in patients with chronic ITP.3 Other studies are under way to evaluate the use of eltrombopag in patients with thrombocytopenia associated with chronic HCV infection and in patients with chemotherapy-induced thrombocytopenia.
ADVERSE EVENTS
Eltrombopag has been very well tolerated in clinical studies to date, with adverse event rates comparable to those observed with placebo.20
In the Bussel et al study,15 the overall incidence of adverse events was similar between patients treated with eltrombopag and those treated with placebo. The incidence of grade 3 or 4 events was 7% among patients treated with eltrombopag 30 mg/d, 13% among patients treated with eltrombopag 50 mg/d, 11% among patients treated with eltrombopag 75 mg/d, and 14% among patients who received placebo. Headache was the most common side effect noted in the treatment groups (range, 10%–21%). Other side effects reported with eltrombopag treatment included aspartate aminotransferase (AST) elevation (range, 3%–7%), constipation (range, 3%–7%), fatigue (range, 3%–7%), rash (range, 3%–7%), anemia (3%–4%), diarrhea (4%), peripheral edema (range, 3%–4%), taste disturbance (4%), abdominal distention (3%), arthralgia (3%), epistaxis (13%), and pain in the extremities (7%). Because of the sample size of this study, an incidence of 3% to 4% correlates to 1 patient. The grade 3 or 4 toxicities reported by patients in the 3 treatment groups included leg pain, pneumonitis, rectal hemorrhage, herpes zoster, thrombocytopenia, pneumonia, hepatitis, renal failure, chronic obstructive pulmonary disease (COPD), trigger finger, menorrhagia, and rash. One death occurred in the study; the patient experienced pneumonia, hepatitis, renal insufficiency, and a COPD exacerbation and died of cardiopulmonary failure on Day 25 of the study. One cataract progression occurred at 181 days poststudy in a patient who had received 8 days of treatment with eltrombopag.
In the EXTEND trial, adverse drug-related events were reported in 32% of patients.19 The most common adverse event was headache (20%). Overall, 13% of patients reported serious adverse events. Two deaths were reported, but they were determined not to be related to the study drug.
Prolonged platelet count elevation was reported in 2 patients in clinical trials.21 Both affected patients were Asian women. One patient was aged 79 years and had a baseline platelet count of 26,000/mm3. Fifteen days after initiation of eltrombopag therapy, the drug was discontinued because the patient's platelet count reached 591,000/mm3. The platelet count peaked at 664,000/mm3 on Day 22, and at Day 85, her platelet count was 116,000/mm3. The second patient was aged 49 years and had a baseline platelet count of 69,000/mm3. Fifteen days after initiation of eltrombopag therapy, the drug was discontinued because the patient's platelet count reached 283,000/mm3 (peak count). At Day 85, her platelet count was 111,000/mm3.
The REPEAT study reported data on adverse events associated with ≥6 weeks of therapy.17 The most commonly reported adverse event was headache (17%). Interestingly, the level of thrombocytopenia was evaluated during the off-periods of this study. Investigators noted that 5 of 66 patients developed platelet counts <10,000/mm3 and 13 of 66 patients developed platelet counts <20,000/mm3 during these periods. This transient thrombocytopenia was not associated with increased bleeding risk.
Based on the studies available, eltrombopag appears to be well tolerated, with headache being the most commonly reported adverse event. Other adverse events appear to be relatively uncommon, with incidence rates similar to those observed with placebo. Ocular adverse events have not been observed in early trials, but continued monitoring for these events is warranted, particularly as long-term use of eltrombopag is studied; early animal studies indicated ocular toxicity.
Because of the relatively small number of patients exposed to eltrombopag to date and the lack of long-term data, the manufacturer has proposed a RiskMAP system to address issues of long-term safety and efficacy. If eltrombopag is approved, the RiskMAP program would include mandatory enrollment of prescribers and patients, controlled distribution, follow-up and monitoring, and education for prescribers and patients.3
DRUG INTERACTIONS
Currently, limited data exist regarding drug interactions with eltrombopag. Investigators have evaluated the bioavailability of eltrombopag when the agent is administered with antacids and high-fat meals. When eltrombopag is administered with a high-fat meal containing calcium or with a polyvalent cation-containing antacid, the plasma concentrations of eltrombopag are significantly decreased. This effect was not observed when eltrombopag was administered with a meal low in calcium content (<50 mg), regardless of the fat content. Taking eltrombopag without food or with a low-calcium meal and separately from antacids may therefore maximize the concentration of the agent.3
In healthy adults, eltrombopag has been demonstrated to inhibit OATP1B1 and to increase rosuvastatin Cmax levels 2-fold.3
Because this agent does not interact with CYP enzymes, eltrombopag administration should not affect drugs that are metabolized through this system.3
DOSING AND ADMINISTRATION
Eltrombopag is still pending FDA approval; definitive chronic dosing in patients has not yet been established. Based on trials in patients with chronic ITP, a dose of 50 mg/d for up to 6 weeks of therapy should be adequate to produce platelet counts >50,000/mm3.15,19 An initial increase in platelet counts should begin within 8 days of therapy initiation. Study results have not demonstrated higher efficacy rates with eltrombopag 75 mg/d in this patient population.15,19 Because of the high incidence of platelet counts >200,000/mm3 that occurs with eltrombopag treatment, platelet counts should be checked frequently during treatment. If platelet counts increase to >200,000/mm3, therapy should be discontinued and platelet counts should be monitored. It is unclear if and when therapy should be restarted; however, the most prudent approach would be to monitor the patient for bleeding and for the morbidity and mortality associated with lower platelet counts. If thrombocytopenia recurs, a second course of therapy should be considered, although the agent should be used cautiously. On the basis of data from the EXTEND and REPEAT trials, it may be reasonable to consider cyclical treatment with periods of no drug use to manage ITP for longer periods of time.16,17,19
Dr Skirvin is an associate clinical professor, Bouvé College of Health Sciences, School of Pharmacy, Northeastern University, Boston, Massachusetts.
Disclosure Information: The author reports no financial disclosures as related to products discussed in this article.
REFERENCES
1. Stasi R, Evangelista ML, Stipa E, Buccisano F, Venditti A, Amadori S. Idiopathic thrombocytopenia purpura: Current concepts in pathophysiology and management. Thromb Haemost. 2008;99:4–13.
2. Schwartz RS. Immune thrombocytopenia purpura-from agony to agonist. N Engl J Med. 2007; 357:2299–2301.
3. FDA Oncologic Drug Advisory Committee. Promacta (Eltrombopag tablets). http://www.fda.gov/ohrms/dockets/ac/08/briefing/2008-4366b1-02-GSK.pdf.
4. Godeau B, Chevret S, Varet B, et al; for the French AITP study group. Intravenous immunoglobulin or high-dose methylprednisolone, with or without oral prednisone, for adults with untreated severe autoimmune thrombocytopenic purpura: A randomised, multicentre trial. Lancet. 2002;359:23–29.
5. Newman GC, Novoa MV, Fodero EM, Lesser ML, Woloski BMR, Bussel JR. A dose of 75 mcg/kg/d of i.v. anti-D increase the platelet count more rapidly and for a longer period of time than 50 mcg/kg/d in adults with immune thrombocytopenic purpura. Br J Haematol. 2001;112:1076–1078.
6. Kojouri K, Vesely SK, Terrell DR, George JN. Splenectomy for adult patients with idiopathic thrombocytopenic purpura: A systematic review to assess long-term platelet count responses, prediction of response, and surgical complications. Blood. 2004; 104:2623–2634.
7. Braendstrup P, Bjerrum OW, Nielsen OJ, et al. Rituximab chimeric anti-CD20 monoclonal antibody treatment for adult refractory idiopathic thrombocytopenic purpura. Am J Hematol. 2005; 78:275–280.
8. FDA approves romiplostim (Nplate) for the treatment of thrombocytopenia. FDA website. http://www.fda.gov/cder/offices/oodp/whatsnew/romiplostim.htm. Accessed September 25, 2008.
9. Nplate [package insert]. Thousand Oaks, CA: Amgen Inc; 2008.
10. Kuter DJ. New thrombopoietic growth factors. Blood. 2007;109: 4607–4616.
11. Stasi R, Evangelista ML, Amadori S. Novel thrombopoietic agents: A review of their use in idiopathic thrombocytopenia purpura. Drugs. 2008;68:901–912.
12. Jenkins JM, Williams D, Deng Y, Uhl J, et al. Phase 1 clinical study of eltrombopag, an oral, nonpeptide thrombopoietin receptor agonist. Blood. 2007; 09:4739–4741.
13. Psaila B, Bussel JB, Linden MD, et al. In vivo effects of eltrombopag on human platelet function. Blood (ASH Annual Meeting Abstracts). 2007;110. Abstract 1301.
14. Psaila B, Villarica G, Bussel JB. Insights into therapeutic mechanisms: Measuring immature platelet fraction (IPF) describes response to treatment in immune thrombocytopenic purpura (ITP). Blood (ASH Annual Meeting Abstracts). 2006;108. Abstract 1070.
15. Bussel JB, Cheng G, Saleh MN, et al. Eltrombopag for the treatment of chronic idiopathic thrombocytopenia purpura. N Engl J Med. 2007;357:2237–2247.
16. Bussel JB, Cheng G, Mansoor S, et al. Long-term safety and efficacy of oral eltrombopag for the treatment of idiopathic thrombocytopenic purpura (ITP). Presented at: 13th Congress of the European Hematology Association; June 12–15, 2008; Copenhagen, Denmark. Abstract 0949.
17. Psaila B, Bussel J, Vasey S, et al. Efficacy and safety of repeated intermittent treatment with eltrombopag in patients with chronic idiopathic thrombocytopenic purpura (ITP). Presented at: 13th Congress of the European Hematology Association; June 12–15, 2008; Copenhagen, Denmark. Abstract 0294.
18. Bussel JB, Cheng G, Saleh M, et al. Analysis of bleeding in patients with immune thrombocytopenic purpura (ITP): A randomized, double-blind, placebo-controlled trial of eltrombopag, an oral platelet growth factor. Blood (ASH Annual Meeting Abstracts). 2006;108. Abstract 475.
19. Bussel JB, Cheng G, Kovaleva L, et al. Long-term safety and efficacy of oral eltrombopag for the treatment of subjects with idiopathic thrombocytopenic purpura (ITP): Preliminary data from the EXTEND study. Blood (ASH Annual Meeting Abstracts). 2007:110. Abstract 566.
20. Bussel JB, McHutchison J, Provan D, Jagiello-Gruzfeld A, Rafi R, Goodison S. Safety of eltrombopag, an oral non-peptide platelet growth factor, in the treatment of thrombocytopenia: Results of four randomized, placebo-controlled studies. Blood (ASH Annual Meeting Abstracts). 2007;110. Abstract 1299.
21. Cheng G. Platelet counts remain elevated in two patients with idiopathic thrombocytopenic purpura after cessation of oral eltrombopag. Blood (ASH Annual Meeting Abstracts). 2007;110. Abstract 3927.
Employers Face Barriers With Adopting Biosimilars
March 1st 2022Despite the promise of savings billions of dollars in the United States, adoption of biosimilars has been slow. A roundtable discussion among employers highlighted some of the barriers, including formulary design and drug pricing and rebates.
