- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Etravirine: A non-nucleoside reverse transcriptase inhibitor for the treatment of resistant HIV-1 infection
Etravirine is a second-generation non-nucleoside reverse transcriptase inhibitor (NNRTI) that was approved January 18, 2008, for use in combination with other antiretroviral agents for the treatment of HIV-1 infection in antiretroviral treatment-experienced adult patients who have evidence of viral replication and HIV-1 strains resistant to NNRTIs and other antiretroviral agents.
Abstract
Etravirine is a second-generation non-nucleoside reverse transcriptase inhibitor (NNRTI) that was approved by FDA on January 18, 2008, for use in combination with other antiretroviral agents for the treatment of HIV-1 infection in antiretroviral treatment-experienced adult patients who have evidence of viral replication and HIV-1 strains resistant to NNRTIs and other antiretroviral agents. Etravirine has a flexible structure that allows multiple binding configurations, making this agent active against wild-type HIV-1 viral strains and against viral strains with known NNRTI resistance mutations. In clinical trials, etravirine has been associated with significant reductions in HIV-1 RNA viral loads in antiretroviral-naïve and antiretroviral-experienced patients. Etravirine is generally well tolerated. The most common adverse event is a mild rash that usually occurs during the second week of therapy and resolves with continued therapy. Although rare, etravirine has been associated with severe skin reactions, including Stevens-Johnson syndrome. Etravirine's broad spectrum of activity and twice-daily dosing schedule help make this agent a valuable treatment option for patients with HIV-1 infection who have developed resistance to other NNRTIs. (Formulary. 2008; 43:105–114.)
An estimated 33.2 million individuals worldwide and 1.3 million individuals in North America are living with HIV, and as many as 27% of these individuals are undiagnosed and unaware of their infection.1 It is estimated that >40,000 new cases of HIV infection are reported in North American adults and adolescents annually.1
Non-nucleoside reverse transcriptase inhibitors (NNRTIs), such as efavirenz, nevirapine, and delavirdine, are an important component of first-line antiretroviral therapy, as these agents have demonstrated efficacy in treating HIV-1 infection. The Department of Health and Human Services' treatment guidelines recommend that treatment-naïve patients receive an NNRTI or protease inhibitor (PI) plus a preferred combination of nucleoside reverse transcriptase inhibitors (NRTIs).2 Development of drug resistance is a major limitation to treatment with currently available NNRTIs, and a single amino acid substitution can create cross-resistance; thus, prior to the development of etravirine, NNRTIs were restricted to use in treatment-naïve patients.3,4
Etravirine (Intelence, Tibotec) is a potent second-generation NNRTI with broad in vitro activity against HIV-1. Etravirine was approved by FDA on January 18, 2008, for use in combination with other antiretroviral agents for the treatment of HIV-1 infection in antiretroviral treatment-experienced adult patients who have evidence of viral replication and HIV-1 strains resistant to NNRTIs and other antiretroviral agents.5
CHEMISTRY AND PHARMACOLOGY
Etravirine (4-[[6-amino-5-bromo-2-[(4-cyanophenyl)amino]-4-pyrimidinyl]oxy]-3,5-dimethylbenzonitrile) is a diarylpyrimidine (DAPY) NNRTI.6 NNRTIs bind directly to the reverse transcriptase enzyme, preventing the conversion of viral RNA into DNA. Etravirine binds to the reverse transcriptase enzyme via a horseshoe-shaped configuration with 2 "wings" capable of rotating to optimize binding.7 This structure allows for multiple binding conformations and may explain etravirine's potent activity against NNRTI-resistant strains.6,7 Although not clinically relevant, etravirine has demonstrated activity against HIV-2, reflecting the agent's broad spectrum of activity.6 The 50% effective concentration (EC50) for etravirine against wild-type HIV-1 is in the nanomolar range (1.4–4.8 nM), which is similar to that of efavirenz (1.0–3.4 nM).6,7
RESISTANCE ANALYSIS
All patients who receive NNRTIs will inevitably develop resistance to the treatment, and when resistance develops, currently available agents are ineffective as part of an antiretroviral regimen. This resistance can develop rapidly (eg, after a single dose of nevirapine) or gradually, over several weeks.8 The majority of etravirine trials have focused on patients with NNRTI-resistant HIV-1 infections; however, etravirine has also been evaluated as a treatment for patients with wild-type HIV-1 infections.6 In a parallel screening study involving wild-type and NNRTI-resistant HIV-1 strains, etravirine was demonstrated to inhibit 98% of all samples and 97% of NNRTI-resistant strains with an EC50 <100 nM. The investigators concluded that etravirine has a high genetic barrier to resistance with excellent activity against NNRTI-resistant viral strains.6
Using high multiplicity of infection (MOI) studies, investigators have determined that the etravirine resistance pathway is distinct from the pathways of efavirenz and nevirapine resistance, making this agent a potential alternative treatment in patients who have developed resistance to either of these NNRTIs. Etravirine is also associated with delayed selection of resistant mutations from wild-type HIV strains and from HIV strains carrying the K103N and Y181C site-directed mutants. In vitro studies of etravirine demonstrated that L100I, V179F, Y181C, G190E, M230L, and Y318F mutations contribute to etravirine resistance, but ≥2 of these mutations had to be present to confirm resistance.7
In the DUET-1 and DUET-2 clinical trials of etravirine, it was demonstrated that several NNRTI resistance-associated mutations (RAMs) were associated with a decreased response to etravirine. These RAMs were Val90Ile, Leu100Ile, Lys101Glu/Pro, Val 106Ile, Val179Asp/Phe, Tyr181Cys/Ile/Val, and Gly190Ala/Ser. Patients with 0, 1, or 2 RAMS demonstrated a decrease in viral load compared with placebo. The presence of ≥3 RAMs was necessary to substantially decrease the virologic efficacy of etravirine.9,10
Etravirine is active against wild-type and NNRTI-resistant strains of HIV-1; therefore, the agent is suitable for use in patients who have developed resistance to other NNRTIs. Based on the results of the DUET clinical trials, multiple mutations in the reverse transcriptase enzyme are required for the virus to become resistant to etravirine. Therefore, etravirine has a potentially higher genetic barrier to resistance.
PHARMACOKINETICS

Etravirine is extensively protein bound (>99%). In pharmacokinetic studies, steady-state plasma concentration levels were reached within 4 to 6 days of etravirine therapy initiation.8,12
The initial capsule formulation of etravirine was made with polyethylene glycol (PEG) 4000; this formulation was associated with a large pill burden. Patients received approximately 25 g of PEG4000 daily, which, because of its laxative properties, may have caused the gastrointestinal (GI) side effects that some patients experienced.12 Tablet formulations of etravirine that do not contain PEG4000 have since been developed that improve the drug's bioavailability, decrease the pill burden, and improve patient convenience. Scholler et al13 studied the bioavailability of 4 formulations of etravirine versus a reference formulation in healthy individuals. Etravirine tablets that did not contain PEG4000 were associated with a higher maximum plasma concentration (Cmax) and area under the curve (AUC) without a change in the time to (Cmax) (Tmax)
The tablet formulation resulted in a dosing change from 800 mg twice daily to 200 mg twice daily; both the capsule and tablet formulations were used in clinical studies.13
CLINICAL TRIALS

Phase 2a trials. Etravirine was evaluated in two 7-day studies that included both treatment-naïve and treatment-experienced patients.8,12 The first trial included 19 male patients with HIV infection who were antiretroviral naïve.12 These patients were randomized 2:1 to receive etravirine 900 mg monotherapy or placebo twice daily. Etravirine treatment was associated with a statistically significant decrease in mean HIV-1 RNA levels compared with placebo (1.99 vs 0.06 log10 copies/mL; P<.001). The second study included 16 male patients with high-level phenotypic NNRTI resistance and with an HIV-1 RNA viral load >2,000 copies/mL during treatment with ≥2 NRTIs and 1 NNRTI (efavirenz or nevirapine), which was replaced with etravirine 900 mg twice daily.8 After 7 days, the viral load decay rate was 0.13 log10 RNA copies/mL/d (P<.001).
Phase 2b and 3 trials. Several phase 2b and phase 3 trials of etravirine have been conducted. In all of these studies, therapy failure was defined as the presence of infection with HIV containing ≥1 NNRTI resistance-associated mutation and ≥3 primary PI mutations as well as a baseline viral load of either >1,000 or >5,000 copies/mL.9,10,14
The C223 study was a randomized, open-label, partially blinded trial designed to assess the efficacy and safety of 2 dosages of etravirine.14 A total of 199 patients were randomized 2:2:1 to receive etravirine 400 mg or 800 mg twice daily plus ≥2 approved antiretroviral agents (an NRTI and/or lopinavir/ritonavir and/or enfuvirtide) or an active control that consisted of ≥3 antiretroviral agents (NRTIs or PIs and/or enfuvirtide). At the end of 24 weeks, treatment with either dose of etravirine was associated with statistically significant efficacy, demonstrated by the primary end point of change in HIV-1 RNA levels from baseline (mean changes: etravirine 400 mg, –1.04 log10 copies/mL; etravirine 800 mg, –1.18 log10 copies/mL; placebo, –0.19 log10 copies/mL; P<.05 for both etravirine groups vs control). According to 48-week follow-up results, the mean change from baseline in HIV-1 RNA was –1.01, –0.88, and –0.14 log10 copies/mL for patients who received etravirine 800 mg twice daily, 400 mg twice daily, and active control, respectively (P<.05).16 At 48 weeks, a statistically greater proportion of patients had achieved viral loads of <400 copies/mL and <50 copies/mL with etravirine compared with patients who received placebo.16
The DUET-1 and DUET-2 studies were randomized, double-blind, placebo-controlled, continuing phase 3 trials of etravirine that included patients who were developing resistance to their current antiretroviral therapy.9,10 Patients were randomized 1:1 to receive etravirine 200 mg twice daily or placebo. All patients also received darunavir 600 mg/ritonavir 100 mg twice daily, investigator-selected NRTIs, and/or enfuvirtide; treatment was based on screening genotype resistance patterns. The primary end point in both trials was the proportion of participants who achieved an HIV viral load of <50 copies/mL at Week 24. Secondary end points included changes in viral load and CD4+ count from baseline and safety analyses.
Results from the DUET-1 study, which evaluated 612 patients, demonstrated statistical significance in favor of etravirine treatment in all predetermined measures of efficacy.9 At Week 24, 56% of patients who received etravirine and 39% of patients who received placebo achieved viral loads <50 copies/mL (response rate difference, 17%; 95% CI, 9%–25%; P=.005).
The DUET-2 study evaluated 591 patients. The trial yielded efficacy data similar to those from the DUET-1 study: 62% of patients who received etravirine and 44% of patients who received placebo achieved viral loads <50 copies/mL at Week 24 (response rate difference, 18%; 95% CI, 11%–26%; P=.0003). The reported adverse events were generally similar among patients who received etravirine and those who received placebo. The incidence of adverse events was also similar between the DUET-1 and DUET-2 trials; however, the use of etravirine was associated with a greater incidence of a rash in the DUET-1 trial compared with the DUET-2 trial. In the DUET-2 trial, 14% of patients who received etravirine reported a rash of any type compared with 9% of patients who received placebo (P=.0723.) In the DUET-1 trial, 20% of patients who received etravirine reported a rash of any type compared with 10% of patients who received placebo (P<.0001).
Pooled results from the DUET-1 and DUET-2 trials have also been made available; the data are similar to those from the individual DUET trials.15 In this pooled-data report, the combined primary end point of the proportion of patients with HIV viral load <50 copies/mL was 59% versus 41% among patients treated with etravirine and placebo, respectively (P<.0001).
The full 48-week results of the DUET-1 and DUET-2 trials have not yet been released; however, initial results are promising.17
ADVERSE EVENTS
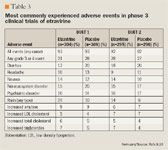
In the DUET trials, etravirine was generally well tolerated, with overall adverse reactions comparable to those observed with placebo (Table 3).9,10,15 The most significant adverse event reported during clinical studies was the development of an erythematous or maculopapular rash, which occurred in 17% of patients who received etravirine versus 9% of patients who received placebo (pooled data; P=.0001).15 The rash generally appeared during the second week of treatment and resolved with continued therapy. The majority of adverse events (98.7%) were mildly to moderately severe and resulted in discontinuation of treatment among only 2.2% of patients. 15 In rare cases, patients who received etravirine developed severe skin reactions, including hypersensitivity, erythema multiforme, and Stevens-Johnson syndrome. More women experienced a rash than men (28% vs 16%); however, there were no sex-related differences in the severity of the rash or in discontinuation rates.15 Patients who have a history of an NNRTI-associated rash do not appear to be predisposed to developing an etravirine-associated rash.9,10
DRUG INTERACTIONS
Etravirine is metabolized by CYP3A4, CYP2C9, and CYP2C19.5,11,18 CYP3A4 is thought to be a minor metabolic pathway.

EDITORS' NOTE:
A full listing of changes in the pharmacokinetic concentrations of etravirine and co-administered drugs when the agents are used concomitantly is available at http://www.formularyjournal.com/.
DOSING AND ADMINISTRATION
The recommended dose of etravirine is 200 mg (two 100-mg tablets) twice daily after a meal.5,9,10 Information regarding etravirine dosing in special populations is limited. As such, etravirine should be used with caution in patients who are pregnant or have significant organ dysfunction.
PRICING
The average wholesale price (AWP) for 120 tablets of etravirine 100 mg (1-mo supply) is $654; this translates to a daily cost of $21.80.33
REFERENCES
1. Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization (WHO). AIDS epidemic update: December 2007. data.unaids.org/pub/epislides/2007/2007_epiupdate_en.pdf. Accessed February 15, 2008.
2. Department of Health and Human Services. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. http://www.aidsinfo.nih.gov/contentfiles/adultandadolescentgl.pdf. Published January 29, 2008. Accessed February 15, 2008.
3. Demeter LM, Shafer RW, Meehan PM, et al. Delavirdine susceptibilities and associated reverse transcriptase mutations in human immunodeficiency virus type 1 isolates from patients in a phase I/II trial of delavirdine monotherapy (ACTG 260). Antimicrob Agents Chemother. 2000;44:794–797.
4. Richman DD, Havlir D, Corbeil J, et al. Nevirapine resistance mutations of human immunodeficiency virus type 1 selected during therapy. J Virol. 1994;68:1660–1666.
5. Intelence [package insert]. Raritan, NJ: Tibotec, Inc; 2008.
6. Vingerhoets J, Azijn H, Fransen E, et al. TMC125 displays a high genetic barrier to the development of resistance: Evidence from in vitro selection experiments. J Virol. 2005;79:12773–12782.
7. Andries K, Azijn H, Thielemans T, et al. TMC125, a novel next-generation nonnucleoside reverse transcriptase inhibitor active against nonnucleoside reverse transcriptase inhibitor-resistant human immunodeficiency virus type 1. Antimicrob Agents Chemother. 2004;48:4680–4686.
8. Gazzard BG, Pozniak AL, Rosenbaum W, et al. An open-label assessment of TMC 125-a new, next-generation NNRTI, for 7 days in HIV-1 infected individuals with NNRTI resistance. AIDS. 2003;17:F49–F54.
9. Madruga JV, Cahn P, Grinsztejn B, et al; for the DUET-1 Study Group. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1-infected patients in DUET-1: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet. 2007;370:29–38.
10. Lazzarin A, Campbell T, Clotet B, et al; for the DUET-2 Study Group. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1-infected patients in DUET-2: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet. 2007;370:39–48.
11. Haslinger BA, Arendt G. TMC-125 Tibotec. Curr Opin Investig Drugs. 2004;5:208–213.
12. Boffito M, Winston A, Jackson A, et al. Pharmacokinetics and antiretroviral response to darunavir/ritonavir and etravirine combination in patients with high-level viral resistance. AIDS. 2007;21:1449–1455.
13. Gruzdev B, Rakhmanova A, Doubovskaya E, et al. A randomized, double-blind, placebo-controlled trial of TMC125 as 7-day monotherapy in antiretroviral naive, HIV-1 infected subjects. AIDS. 2003;17:2487–2494.
14. Scholler M, Hoetelmans R, Beets G, et al. Substantial improvement of oral bioavailability of TMC125 using new tablet formulations in healthy volunteers [abstract]. Presented at: The 3rd International AIDS Society (IAS) Conference on HIV Pathogenesis and Treatment; July 24–27, 2005; Rio de Janeiro, Brazil. Abstract TUPE.1±1.
15. Nadler JP, Berger DS, Blick G, et al; The TMC125-C223 Writing Group. Efficacy and safety of etravirine (TMC125) in patients with highly resistant HIV-1: Primary 24-week analysis. AIDS. 2007;21:F1–F10.
16. Cohen C, Steinhart CR, Ward DJ, et al. Efficacy and safety results at 48 weeks with the novel NNRTI, TMC125, and impact of baseline resistance on the virologic response in study TMC125-C223 [abstract]. Presented at: The XVI International AIDS Conference; August 13–18, 2006; Toronto, Canada. Abstract TUPE0061.
17. Cahn P, Haubrich R, Leider J, et al; for the DUET-1 and DUET-2 study groups. Pooled 24-week results of DUET-1 and DUET-2: TMC125 (etravirine; ETR) versus placebo in treatment-experienced HIV-1-infected patients [abstract]. Presented at: The 47th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC); September 17–20, 2007; Chicago, IL. Abstract H-717.
18. New 48-week efficacy and safety data presented for INTELENCE (etravirine) as part of HIV combination therapy [press release]. Boston, MA: Tibotec Therapeutics; February 7, 2008.
19. Schöller-Gyüre M, Woodfall B, De Marez, et al. Pharmacokinetics of TMC125, with atazanavir (ATV) and atazanavir/ritonavir (ATV/r) [abstract]. Presented at: The Eighth International Congress on Drug Therapy in HIV Infection; November 12–16, 2006; Glasgow, UK. Abstract 56.
20. LP Protocol A40010410, Tibotec Therapeutics, July 2007; 1–4 (data on file).
21. Schöller-Gyüre M, Woodfall B, Bollen S, et al. Pharmacokinetics of amprenavir and TMC125 in HIV-infected volunteers receiving TMC125 with fosamprenavir/ritonavir [abstract]. Presented at: The 46th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC); September 27–30, 2006; San Francisco, CA. Abstract A-370.
22. Schöller-Gyüre M, Debroye C, Woodfall B, et al. Pharmacokinetic interaction between TMC125 and clarithromycin [abstract]. Presented at: The 44th Annual Meeting of the Infectious Diseases Society of America (IDSA); October 12–15, 2006; Toronto, Canada. Abstract 962.
23. Schöller, Kraft M, Hoetelmans R, et al. Significant decrease in TMC125 exposures when co-administeredwith tipranavir (boosted with ritonavir) in healthy subjects [abstract]. Presented at: The 13th Conference on Retroviruses and Opportunistic Infections (CROI); February 5–9, 2006; Denver, CO. Abstract 583.
24. Schöller M, Hoetelmans R, Bollen S, et al. No significant interaction between TMC125 and didanosine (ddI) in healthy volunteers [abstract]. Presented at: The 3rd International AIDS Society (IAS) Conference on HIV Pathogenesis and Treatment; July 24–27, 2005; Rio de Janeiro, Brazil. Abstract WEPE3.3C16.
25. Schöller-Gyüre M, Debroye C, Woodfall B, et al. Pharmacokinetic evaluation of the interaction between TMC125 and tenofovir disoproxil fumarate [abstract]. Presented at: The 46th Interscience Conference on AntimicrobialAgents and Chemotherapy (ICAAC); September 27–30, 2006; San Francisco, CA. Abstract A-371.
26. Harris M, Zala C, Woodfall B, et al. Pharmacokinetics (PK) and safety of adding TMC125 to stable regimens ofsaquinavir (SQV), lopinavir (LPV), ritonavir (RTV) and NRTIs in HIV+ adults [abstract]. Presented at: The 13th Conference on Retroviruses and Opportunistic Infections (CROI); February 5–9, 2006; Denver, CO. Abstract 575b.
27. Anderson MS, Kakuda TN, Miller JL, et al. Pharmacokinetic evaluation of non-nucleoside reverse transcriptase inhibitor TMC125 and integrase inhibitor raltegravir in healthy volunteers [abstract]. Presented at: The 4th International AIDS Society (IAS) Conference on HIV Pathogenesis, Treatment, and Prevention (IAS); July 22–25, 2007; Sydney, Australia. Abstract TUPDB02.
28. Schöller-Gyüre M, De Smedt G, Vanaken H, et al. TMC125 bioavailability is not affected by ranitidine and omeprazole [abstract]. Presented at: The XVI International AIDS Conference; August 13–18, 2006; Toronto, Canada. Abstract TUPE0082.
29. Schöller-Gyüre M, Woodfall B, Vanaken H,et al. Lack of interaction between TMC125 and methadone [abstract]. Presented at: The XVI International AIDS Conference; August 13–18, 2006; Toronto, Canada. Abstract TUPE0084.
30. Schöller-Gyüre M, Kakuda TN, De Smedt G, et al. Pharmacokinetic interaction between the non-nucleoside reverse transcriptase inhibitor (NNRTI) TMC125 and atorvastatin in HIV-negative volunteers [abstract]. Presented at: The 4th International AIDS Society (IAS) Conference on HIV Pathogenesis, Treatment, and Prevention (IAS); July 22–25, 2007; Sydney, Australia. Abstract WEPEA106.
31. Schöller-Gyüre M, Woodfall B, Debroye C, et al. Pharmacokinetic interaction between TMC125 and Rifabutin [abstract]. Presented at: The 44th Annual Meeting of the Infectious Diseases Society of America (IDSA); October 12–15, 2006; Toronto, Canada. Abstract 963.
32. Schöller-Gyüre M, Debroye C, Aharchi F, et al. No effect of TMC125 on the pharmacokinetics of oral contraceptives [abstract]. Presented at: The Eighth International Congress on Drug Therapy in HIV Infection; November 12–16, 2006; Glasgow, UK. Abstract 57.
33. Tibotec Therapeutics website. Intelence wholesale sell sheet. http://www.intelence-info.com/intelence/assets/pdf/intelence%20wholesale%20sell%20sheet%20-%20english.pdf. Accessed February 18, 2008.
Employers Face Barriers With Adopting Biosimilars
March 1st 2022Despite the promise of savings billions of dollars in the United States, adoption of biosimilars has been slow. A roundtable discussion among employers highlighted some of the barriers, including formulary design and drug pricing and rebates.
