- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Potentially inappropriate medication use in hospitalized older adults: A DUE using the full Beers criteria
The purpose of this drug use evaluation was to report potentially inappropriate medication use, as defined by the full Beers criteria.

Key Points
Abstract
Potentially inappropriate medication (PIM) use in older adults has been associated with increased morbidity. The Beers criteria describe medications that should generally be avoided in older adults. This drug use evaluation (DUE) reports PIM use, as defined by the full Beers criteria including medication, dose, and disease interactions, in 100 hospitalized patients aged ≥65 years. Each patient's home, discharge, and inpatient medication profiles were reviewed. Before admission, 39% of patients were taking ≥1 PIM; this percentage increased significantly to 59% (P<.001 vs before admission) during hospitalization but returned to baseline at discharge (41%; P=.684 vs before admission). Of the 107 active hospital PIM orders, 57% were new and 43% were continued home medications. Pharmacists intervened on only 3 orders. This increased PIM use during hospitalization indicates a need for prescriber and pharmacist education, formulary changes, and alterations to preprinted orders. (Formulary. 2008;43:326–339.)

There have been a variety of studies examining PIM use in older adults as defined by the Beers criteria.11 The rate of PIM use in these studies has ranged from 12.6% to 50%, with the highest PIM use in nursing homes and among frail older adults.5,11 An association between PIM use, as defined by the Beers criteria, and adverse outcomes such as impaired muscle strength and functional status, increased healthcare expenditure, and increased risk of hospitalization and death has been demonstrated.12–14 Lau et al12 demonstrated that PIM use was associated with a 30% increased risk of hospitalization and a 21% increased risk of death in the nursing home setting in frail older adults who were prescribed ≥1 PIM.
A MEDLINE search of peer-reviewed journal articles published from 1997 to 2007 was conducted using the following search terms: elderly, inappropriate medication, drug/disease interaction, and Beers criteria. The search found 4 published studies investigating the use of PIMs, as defined by the Beers criteria, in an inpatient US hospital setting. Three of these studies examined medications administered in the emergency department only and demonstrated rates of PIM use ranging from 12% to 37%.6,15,16 One study evaluated PIM use beyond the emergency department. Bonk et al17 evaluated the administrative database information of 40 University HealthSystem Consortium health centers and found that 50.6% of older adults received ≥1 PIM and 19.4% received ≥2 PIMs during hospitalization. Several studies have demonstrated an association between the use of PIMs, as defined by the Beers criteria, and increased morbidity, including increased hospitalizations, worsened physical function, and poor quality of life.18 However, relatively little is known about the rate of PIM use during hospitalization or the effect that recent hospitalization has on the rate of PIM prescribing. Because most research regarding PIM use has primarily relied on medication or insurance databases, the full Beers criteria, including the drug/disease component, has generally not been examined, nor has the possibility that a PIM may potentially be justified because of patient-specific variables.
The purpose of this DUE was to report PIM use, as defined by the full Beers criteria including medication, dose, and disease interactions, in hospitalized patients aged ≥65 years. Such DUEs may help identify a need for healthcare provider education regarding Beers criteria and safe prescribing in the hospitalized older adult population.
METHODS
This retrospective DUE was conducted at a 760-bed tertiary care teaching hospital. Clinical pharmacy services at this hospital include pharmacy specialists rounding with internal medicine, hospitalist, and surgery/trauma teams, a drug information center, an antibiotic monitoring program, and anticoagulation service. Staff pharmacists perform a variety of clinical services, including intravenous (IV) to oral conversion, dosage adjustments per renal function, ADR reporting, and drug-related laboratory monitoring. All preprinted hypnotic orders contain specialized dosing for patients aged ≥65 years. The pharmacy does not have a clinical service specifically targeted towards medications in older adults.
A convenience sample of 100 patients was selected via a computer-generated list of all patients aged ≥65 years consecutively admitted to a general medical floor beginning April 1, 2006. Patients with a length of stay <3 days were excluded. Data for this DUE were collected from the hospital's integrated computerized patient medication, laboratory, diagnostic, and dictated medical records.
Data on age, sex, attending physician, length of stay, admission date, discharge date, and unit housed were extracted electronically. The home medication list was obtained by screening the dictated history and physical, dictated consults, and the nursing medication admission history. If a home medication list was not available through ≥1 of these avenues, hospital medications ordered on Day 1 of admission were used to determine a likely home medication list. The discharge medication list was obtained from the dictated discharge summary. If the discharge home medication list was unavailable, hospital medications ordered on the last day of admission were evaluated similarly. The inpatient medication list was obtained from the electronic medication administration record. The count of home, hospital, and discharge medications included oral prescription medications, OTC medications, inhalers, and ophthalmics. Multiple types of insulin were counted as a single medication. Double ingredient medications were counted separately; multiple vitamins were counted as a single medication. For the Beers criteria disease interaction screening, the dictated history and physical and discharge summary were the only sources used to obtain disease information.
Each home, discharge, and inpatient medication profile was screened for PIMs appearing on the Beers criteria. Medications administered only during procedures (eg, surgery, catheterization laboratory) were excluded from review. For each identified PIM, the following was determined: actual use and duration of therapy, dosage, frequency, source (continued home medication or a new medication), the prescriber, continuation at discharge, indication for use, and whether the pharmacy department made any recommendations for or against the agent's use.
The PIMs were further divided into potentially justified or deemed to be without justification. Justification for use of a particular PIM included laboratory information, past medical history, medication allergies, and any documentation of other issues, such as failed therapy or compliance problems, that would justify use of that PIM in that particular patient. For example, propoxyphene would be counted as a PIM but would also be included in the count of "potentially justified" PIMs if the particular patient were allergic to other opioids.
The Beers criteria make exceptions for certain PIMs when their use is considered appropriate based on the indication. All such instances were categorized as "appropriate" and were not included in the PIM count, nor were they included in the count of "potentially justified" PIMs. For example, the Beers criteria specify that diphenhydramine is a PIM unless it is being used to treat acute allergic reactions at the lowest dose possible. Therefore, diphenhydramine used as a hypnotic would be counted as a PIM, but diphenhydramine used for the treatment of acute allergic reactions would be considered appropriate.
Data were analyzed using SPSS Statistics version 15.0. Descriptive data were reported using means ± SD or percentages as appropriate. Frequency data were compared using the chi-square test or Fisher's exact test where appropriate. This DUE was approved through expedited review by the Wichita State University and Wichita Medical Research and Education Foundation institutional review boards. This was a noninterventional, retrospective DUE evaluating data that were originally collected solely for nonresearch purposes (diagnosis and treatment); therefore, the institutional review boards determined that prior informed patient consent was not necessary. The DUE was conducted by a clinical pharmacist supervising 4 physician assistant students and a physician assistant. Results were reported to the hospital's pharmacy and therapeutics (P&T) committee.
RESULTS

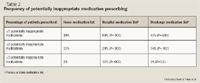
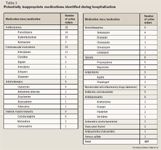
A total of 107 PIMs were identified as active, scheduled, or "as needed" (PRN) orders during hospitalization; however, 27% (29/107) were never administered. Of the 107 PIMs, 43% (46/107) were continued home medications and 57% (61/107) were newly ordered medications (43% were individually written orders and 14% were initiated as part of preprinted, standing orders). Of the 107 PIMs, 74% (79/107) were potentially inappropriate because of the drug ordered, 35% (37/107) were potentially inappropriate because of a disease interaction, and 13% (14/107) were potentially inappropriate because of drug dose. The total exceeds 100% because some medications were potentially inappropriate for multiple reasons; 19% (20/107) were potentially inappropriate because of both the drug ordered and a disease interaction with that drug, and 2.8% (3/107) were potentially inappropriate because of the drug dose and a disease interaction with that drug.
A total of 84% of the PIM orders were categorized as "high risk" according to the Beers criteria, and 16% were categorized as "low risk." Pharmacists intervened on only 3 of the 107 PIM orders; all 3 recommendations were accepted by the prescriber. Of the 107 PIMs identified, 8 (7.5%) were deemed potentially justified. The mean number of PIMs per patient, including all 100 patients, was 1.0±1.20 (range, 0–5). The mean number of PIMs per patient, including only those patients with ≥1 PIM, was 1.8±1.04 (range, 1–5).
DISCUSSION
Limitations. Frequent discrepancies between the home medication lists as dictated in the history and physical, consults, and nursing history were noted. These types of discrepancies in home medication lists occur for a variety of reasons and are not unique to this setting, as previously documented by other researchers.19–21 Inaccuracies in the home or discharge medication list could have altered the count of home and discharge medications and the ability to identify all PIMs. When a home medication list was not available, the first day of admission was used to estimate a likely home medication list: this technique was used for 4% of patients. When a discharge medication list was not available, the last day of admission was similarly used. Unfortunately, the percentage of this occurrence was not recorded. Although every attempt was made to compile accurate lists using clinical reasoning, these cases present the highest likelihood for errors. Similarly, when evaluating the drug/disease component of the Beers criteria, the investigators were unable to screen any diseases not documented in the dictated history and physical or discharge summary. Several conditions on the Beers criteria were nonspecific. For example, "cognitive impairment" as a medical condition required some interpretation to include terms such as dementia, Alzheimer's disease, and organic brain disease. Any disease-state ambiguity was clarified by the physician assistant researcher, and any medication ambiguity was clarified by the pharmacist researcher.
Assessing each PIM to determine whether it was potentially "justified" also required clinical reasoning. PIMs ordered on a PRN basis generally listed an indication for use, allowing for justification to be evaluated. However, indications for scheduled PIMs required review of each patient's past medical history to determine justification.
Prescribers were not contacted individually to discuss rationale for therapy selection. To overcome this limitation and to increase standardization, all PIMs were evaluated by ≥2 of the researchers, one physician assistant student and the clinical pharmacist. Consensus was achieved in all cases. Because the prescribers were not contacted, it is unknown if prescribing PIMs occurred because of a lack of familiarity with the Beers criteria or simply a disagreement with aspects of the criteria. These criteria are based on expert opinion rather than levels of evidence; therefore, the criteria may be open to a wider variety of interpretation than typical evidence-based consensus guidelines.
Clinical implications. A majority of published studies using the Beers criteria to assess prescribing in older adults evaluated lists of prescribed medications only and did not incorporate the patient's past medical history, the drug's indication, the drug's interaction with comorbid conditions, or the potential justification for use of the drug. Several of the Beers criteria require this information to classify the medication as either appropriate or inappropriate; therefore, studies that do not fully evaluate each medication's indication and dose may either overestimate or underestimate PIM use. When comparing a hospital's individual DUE results to published studies, one must take into account these potential differences in methodologies and their effect on variation of findings. Even taking into account individualized potential justification for use, there was a higher than expected rate of PIM use during hospitalization. Increased PIM use in hospitalized older adults may increase the risk of ADRs during hospitalization.
Promethazine and diphenhydramine were 2 of the most commonly prescribed PIMs. More than half of the orders for these 2 drugs originated from preprinted orders: 9 for promethazine and 6 for diphenhydramine. Each of the 9 promethazine orders was prescribed PRN for nausea/vomiting; 1 order was for a 25-mg dose, 5 were for a 12.5-to 25-mg dose, and 3 were for a 12.5-mg dose. According to the Beers criteria, all promethazine use is considered inappropriate in this patient population regardless of dose. However, if promethazine is prescribed, lower dosages are preferable to higher dosages in older adults. Diphenhydramine is considered appropriate for itching if the smallest possible dose is used. Therefore, diphenhydramine orders for 12.5 to 25 mg were considered appropriate. All 6 of the diphenhydramine orders written from preprinted orders were for 25 to 50 mg or for 50 mg PRN for itching. Amiodarone, another frequently prescribed PIM, is associated with a high rate of ADRs even when prescribed at the recommended dosages. It has been recommended that the usual dose of amiodarone should be reduced by 50% in older adults and that this agent should be used only when a clear indication exists.22
Because PIM use puts patients at risk for ADRs, reduction strategies should be implemented whenever possible, and P&T committees may be ideal groups to implement such change. One PIM reduction strategy would be to target hospital preprinted orders. For preprinted orders for medications that are considered inappropriate because of the dose prescribed, a separate line item with a mandatory lower dosage option for patients aged ≥65 years could be added. This strategy has been successfully used to reduce inappropriate hypnotic prescribing in older adults.23 Another strategy is to restrict use of or remove certain drugs from the formulary to help prevent prescribing of those PIMs. Meperidine is no longer considered a first-line analgesic because of its higher rate of central nervous side effects compared with other opioids, and it has been suggested that meperidine should be removed from hospital formularies.24,25 Propoxyphene has minimal efficacy for pain management, similar to that of acetaminophen, yet has the usual side effects associated with opioids plus a high rate of other cardiovascular and central nervous system toxicities, especially in older adults.26 Had these formulary and preprinted order changes been implemented in the 100 patients evaluated in this DUE, PIM use would have been reduced from 59% to 54% (P=.316). This is helpful, but not a statistically significant reduction. Therefore, other reduction strategies must also occur, such as prescriber education regarding the Beers criteria and pharmacist education regarding identification of PIM orders and interception/interventions to alter prescribing patterns. The lack of a formal pharmacy program to address PIM use in older adults likely accounted for the low rate of pharmacy interventions observed in this DUE (2.8%).
Areas for future research. Use of PIMs, as defined by the Beers criteria, has been associated with higher rates of morbidity.18 This DUE did not specifically evaluate the incidence of ADRs. Future DUEs should evaluate the effect that this transient increase in PIM use has on ADR rates during hospitalization. Stronger data may lend stronger support towards implementing policies targeting reduction of PIM prescribing. Little research has been conducted evaluating the use of PIMs in the hospital setting or the effect that hospitalization has on PIM use. The effectiveness of PIM reduction strategies in the hospital setting, including alterations to preprinted orders, formulary changes, and educational interventions, should also be explored. Educational strategies could be expanded to outpatient settings, from which the majority of hospital patients originate. Any PIM reduction strategies implemented during hospitalization may also reduce PIM use after discharge when the patient returns to the outpatient setting.
CONCLUSION
The percentage of patients prescribed ≥1 PIM increased significantly during hospitalization but returned to near baseline at discharge. This increase in PIM use during hospitalization indicates a need for prescriber and pharmacist education, formulary changes, and alterations to preprinted orders.
Dr Hale is an associate professor, Department of Physician Assistant, Wichita State University, Kansas, and a clinical pharmacist, Wesley Medical Center, Wichita, Kansas. Ms Griffin is an assistant professor and clinical supervisor, Department of Physician Assistant, Wichita State University. Ms Cartwright and Mr Moulin are physician assistants, Department of Physician Assistant, Wichita State University. Mr Alford and Mr Fleming are master of physician assistant students, Department of Physician Assistant, Wichita State University.
Disclosure Information: The authors report no financial disclosures as related to products discussed in this article.
REFERENCES
1. Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296:1858–1866.
2. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: A meta-analysis of prospective studies. JAMA. 1998;279:1200–1205.
3. Hanlon JT, Schmader KE, Koronkowski MJ, et al. Adverse drug events in high risk older outpatients. J Am Geriatr Soc. 1997;45:945–948.
4. Lotrich FE, Pollock BG. Aging and clinical pharmacology: Implications for antidepressants. J Clin Pharmacol. 2005;45:1106–1122.
5. Sloane PD, Zimmerman S, Brown LC, Ives TJ, Walsh JF. Inappropriate medication prescribing in residential care/assisted living facilities. J Am Geriatr Soc. 2002;50:1001–1011.
6. Caterino JM, Emond JA, Camargo CA Jr. Inappropriate medication administration to the acutely ill elderly: A nationwide emergency department study, 1992-2000. J Am Geriatr Soc. 2004;52:1847–1855.
7. Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151:1825–1832.
8. Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med. 1997;157:1531–1536.
9. Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: Results of a US consensus panel of experts [erratum in Arch Intern Med. 2004;164:298]. Arch Intern Med. 2003;163:2716–2724.
10. Onder G, Landi F, Cesari M, Gambassi G, Carbonin P, Bernabei R; Investigators of the GIFA Study. Inappropriate medication use among hospitalized older adults in Italy: Results from the Italian Group of Pharmacoepidemiology in the Elderly. Eur J Clin Pharmacol. 2003;59:157–162.
11. Gallagher P, Barry P, O'Mahony D. Inappropriate prescribing in the elderly. J Clin Pharm Ther. 2007;32:113–121.
12. Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Arch Intern Med. 2005;165:68–74.
13. Landi F, Russo A, Liperoti R, et al. Impact of inappropriate drug use on physical performance among a frail elderly population living in the community. Eur J Clin Pharmacol. 2007;63:791–799.
14. Fu AZ, Liu GG, Christensen DB. Inappropriate medication use and health outcomes in the elderly. J Am Geriatr Soc. 2004;52:1934–1939.
15. Budnitz DS, Shehab N, Kegler SR, Richards CL. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med. 2007;147:755–765.
16. Hustey FM, Wallis N, Miller J. Inappropriate prescribing in an older ED population. Am J Emerg Med. 2007;25:804–807.
17. Bonk ME, Krown H, Matuszewski K, Oinonen M. Potentially inappropriate medications in hospitalized senior patients. Am J Health Syst Pharm. 2006;63:1161–1165.
18. Jano E, Aparasu RR. Healthcare outcomes associated with Beers criteria: A systematic review. Ann Pharmacother. 2007;41:438–447.
19. Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: A systematic review. CMAJ. 2005;173:510–515.
20. Nester TM, Hale LS. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. Am J Health Syst Pharm. 2002;59:2221–2225.
21. Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–429.
22. Shetty HG, Woodhouse KW. Use of amiodarone for elderly patients. Age Ageing. 1992;21:233–236.
23. Hale LS, Nester TM. Pharmacy measures to alter hypnotic prescribing in hospitalized elderly [abstract]. J Kansas Pharm. 2001;75:15.
24. O'Connor AB, Lang VJ, Quill TE. Eliminating analgesic meperidine use with a supported formulary restriction. Am J Med. 2005;118:885–889.
25. Beckwith MC, Fox ER, Chandramouli J. Removing meperidine from the health-system formulary-frequently asked questions. J Pain Palliat Care Pharmacother. 2002;16:45–59.
26. Barkin RL, Barkin SJ, Barkin DS. Propoxyphene (dextropropoxyphene): A critical review of a weak opioid analgesic that should remain in antiquity. Am J Ther. 2006;13:534–542.
Employers Face Barriers With Adopting Biosimilars
March 1st 2022Despite the promise of savings billions of dollars in the United States, adoption of biosimilars has been slow. A roundtable discussion among employers highlighted some of the barriers, including formulary design and drug pricing and rebates.
