- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
A review of the prevention and treatment of venous thromboembolism
Venous thromboembolism (VTE) is a debilitating and potentially fatal condition, often seen in the aging population. VTE results from clot formation in the venous circulation and presents as either deep-vein thrombosis or pulmonary embolism. A population-based study estimated that at least 201,000 new cases of VTE occur in the United States annually.

Key Points
Abstract
Venous thromboembolism (VTE) is a debilitating and potentially fatal condition, often seen in the aging population. VTE results from clot formation in the venous circulation and presents as either deep-vein thrombosis (DVT) or pulmonary embolism (PE). A population-based study estimated that at least 201,000 new cases of VTE occur in the United States annually. Of these, 107,000 are DVT cases, while the remaining 94,000 present as PE. The goals for acute treatment of DVT are to prevent further clotting, prevent acute pulmonary emboli, reduce the risk of recurrent thrombosis, and to truncate the development of complications including venous insufficiency and post-thrombotic syndrome. Patients with acute DVT should be treated with one of several therapies. These include subcutaneous (SC) low-molecular-weight heparin, intravenous unfractionated heparin (UFH), SC UFH with monitoring, fixed-dose SC UFH, or SC fondaparinux, versus no treatment at all. (Formulary. 2010. 45:91–100.)
Venous thromboembolism (VTE) is a debilitating and potentially fatal condition, often seen in the aging population. VTE results from clot formation in the venous circulation and presents as either deep-vein thrombosis (DVT) or pulmonary embolism (PE). Some cases of VTE may be asymptomatic, and others are evident only after sudden death because of PE. Often, patients have both DVT and PE, one of which may be subclinical.1 Since acute treatment for DVT and PE are the same, further clinical examination is not warranted once diagnosis of the symptomatic presentation is made.
RISK FACTORS
Several risk factors are associated with the development of VTE. In a review of 1,231 patients with VTE, 96% of these patients had one or more risk factors.4 Risk of VTE is cumulative, increasing proportionally to the number of potential contributing factors one has. These include increased age, previous episode of VTE, prolonged immobility, malignancy, trauma, major surgery, hypercoagulable state, and estrogen-containing medications.4 Perhaps the greatest risk factor is a history of VTE, most likely because of damage to the vessels and obstruction of blood flow caused by the initial embolism. The cumulative incidence rate of recurrent VTE increased from 7% after 1 year to approximately 22% after 5 years of the initial event.5 The risk of recurrent VTE is increased within the first 6 to 12 months, but can persist for at least 10 years after the initial event.6 Nineteen percent of the patients with VTE had at least 1 prior episode of VTE.4 Additionally, the Duration of Anticoagulation Study concluded the 2-year incidence rate was 18% in patients anticoagulated for 6 weeks but only 9.5% in patients treated for 6 months.7
Major surgery is the most studied and well-known risk factor for development of VTE and encompasses thoracic, abdominal, and orthopedic surgeries. Lower-extremity orthopedic procedures carry the highest risk. Approximately half of patients who undergo elective knee or hip replacement without prophylaxis will develop VTE.4 Orthopedic fractures also are associated with an increased risk of VTE development.
VTE is a common complication of cancer. The risk associated with major surgery is increased 2 to 3 times if it is to treat malignancy.4,8 It is estimated that 1 in every 200 cancer patients will experience VTE.8 Moreover, patients who are diagnosed with idiopathic DVT or PE often are subsequently diagnosed with cancer. The mechanism behind this is not entirely clear. It is thought that tumor cells release substances that activate the coagulation cascade while also decreasing levels of protein C, protein S, and antithrombin, thereby promoting a procoagulant effect.9 VTE occurs most often with cancers of the pancreas, lung, stomach, prostate, breast, and in adenocarcinomas of unknown origin.8
Hereditary conditions. Several hereditary conditions or gene mutations lead to a hypercoagulable state. Most often, thrombosis develops in patients with such conditions after another risk factor is added, such as prolonged immobility, initiation of estrogen-containing contraceptives, or major surgery. The most common inherited disorder inducing a hypercoagulable state is activated protein C resistance. One such example is factor V Leiden, a mutation of intrinsic factor V that causes resistance to protein C. This condition is seen in 5% of Caucasians and 1% of African-Americans, but is absent in Asians.10 Patients with factor V Leiden have a 2- to 3-fold risk of developing VTE compared with patients without this mutation.4,10
Antiphospholipid antibody syndrome, which is further divided into the lupus anticoagulant syndrome and the anticardiolipin syndrome, is the most common hypercoagulable state and can be inherited or induced by the use of some medications (phenytoin, quinidine, hydralazine, and quinine, for example).10 Anticardiolipin syndrome is 5 times more likely to occur than lupus anticoagulant syndrome; however, both significantly increase the risk of thrombosis.4,10
Although less common, inherent deficiencies of the natural anticoagulants protein C, protein S, and antithrombin can also increase the risk of thrombosis. The relative risk for developing thrombosis is 7.3 with protein C deficiency, 8.5 with protein S deficiency, and 8.1 with antithrombin deficiency.10
The association between VTE and estrogen-containing contraceptives has been well known since as early as the 1960s. Risk of VTE is increased when estrogen is used as either a contraceptive or in hormone replacement therapy. Additional evidence has since shown that the progestins used in combination oral contraceptives can also affect the risk of thrombosis.11 Recent studies have shown a 2- to 6-fold increase in the risk of VTE in oral contraceptive (OCP) users and a 2- to 4-fold increased risk in hormone replacement users.10,11 Although the exact mechanism for this increase is unknown, it is thought that estrogen increases serum clotting factors and induces activated protein C resistance.9 The risk for thrombosis in OCP users is highest in the first year of use, suggesting yet another possible mechanism and is also significantly increased in OCP users who smoke and are aged >35 years.11 Increased serum estrogen levels seen in pregnancy and the immediate postpartum state may also explain the increased VTE risk.
Immobility leading to venous stasis contributes to VTE formation. In recent years, special attention has been paid to the risks of VTE associated with long-duration air travel. This is commonly known as "economy class syndrome." A trial found that approximately 10% of travelers on flights lasting more than 8 hours developed asymptomatic DVT.12 The longer the duration of travel, the higher the risk is of developing PE.13 The clinical significance of this risk, however, remains low, and thromboprophylaxis is not routinely recommended unless a patient is at an already high risk for VTE.4 Regardless, it may be beneficial to recommend simple precautions such as frequent leg movements, chair exercises, and hydration to all long-distance air travelers.4,12,13
PATHOPHYSIOLOGY
Hemostasis, the cessation of bleeding after vascular injury, is a critical yet complex regulatory function of the human body, and it is essential in maintaining balance between hemorrhage and clotting. Abnormalities in the factors needed to maintain hemostasis can lead to bleeding or thrombotic disorders. The blood vessel walls, speed of blood flow, and blood clotting factors, together known as Virchow's Triad, have an important role in thrombosis formation. Abnormalities in any of the elements in the triad may lead to the formation of clots.
Blood flows through the venous system slowly. In the deep veins of the lower extremities, this is particularly true. Valves in these blood vessels, as well as contractions of the calf and thigh muscles, allow the flow of blood back to the heart and lungs. Damage to the valves, or long periods without muscle contraction, leads to venous stasis which in turn reduces the clearance of activated clotting factors and influx of regulatory enzymes through the vessel.9,14–16
The regulation of coagulation in the body is a complex pathway with several enzymes involved. Normally, the blood vessel walls secrete a number of substances that prevent platelet adhesion, activation of clotting factors, and fibrin formation, thus maintaining the smooth flow of blood. When vascular injury occurs, platelets bind to von Willebrand factor and then adhere to the glycoprotein Ib receptors on the subendothelium. The platelets are then activated and glycoprotein IIb/IIIa receptors are formed on the platelet wall; the platelets are now able to adhere together using fibrinogen to form an aggregate. The aggregated platelets then activate the extrinsic pathway of the clotting cascade, producing thrombin. Thrombin (factor IIa) is responsible for the conversion of fibrinogen (factor I) to fibrin (factor Ia), which more securely binds the aggregated platelets. Besides enhancing platelet aggregation due to the conversion of fibrinogen to fibrin and interacting with the glycoprotein IIb/IIIa receptors, thrombin also converts factors V and VIII to their active forms. By activating factors V and VIII, a positive feedback loop is created, leading to more thrombin production. Thrombin is a key component of the coagulation process.9,14–16
Clotting factors are regularly circulating in the blood in their inactive forms. Once activated, the factor then converts the next precursor in the sequence, hence the term "coagulation cascade." The coagulation cascade is traditionally divided into 3 pathways: extrinsic, intrinsic, and common.9 The extrinsic pathway is the principal trigger for the coagulation cascade and is also known as the tissue factor pathway. The final steps of the entire cascade are the conversion of prothrombin to thrombin and fibrinogen to fibrin. Pharmacologic agents currently available to treat and prevent VTE act to ultimately prevent the formation of thrombin.
DIAGNOSIS OF DVT
When considering DVT as a diagnosis, it is important to recognize that upper-extremity DVT pathogenesis differs from that of lower-extremity DVT. This article focuses on DVT of the lower extremities. Lower-extremity DVT can be either distal (anterior tibial veins, posterior tibial veins, peroneal veins) or proximal (popliteal, femoral, or iliac veins).15
In studies evaluating embolic risk and utility of diagnostic testing, it has been observed that proximal DVT is considered of higher clinical importance due to an increased risk of fatality with thrombosis in this region.17,18 Nearly a quarter to half of patients with proximal DVT can be diagnosed via noninvasive testing.17,18 As discussed above, patients that present with proximal DVT may have a silent PE. Up to 40% of patients in 1 study were diagnosed with silent, asymptomatic PE after presenting with symptoms of proximal DVT in subsequent lung scans.19
Distal DVT is therefore of lesser clinical importance, but still presents high risk for the untreated patient. The risk of thrombosis extension in these patients is elevated if not properly anticoagulated. This proximal extension can lead to pulmonary embolus and associated risk of morbidity and mortality.20,21
Although a serious consideration in the patient presenting with symptoms of DVT, the presence of DVT is clinically less common than may be suspected, and only a minority of patients will require anticoagulation.20,21 However, because of the potential risks of undiagnosed DVT (including fatal PE) and associated risks of giving a patient unnecessary anticoagulation (including fatal bleeding), it is essential to properly diagnose the disease with accepted treatment algorithms and objective testing measures.22
The aforementioned risk factors accompanied by common symptoms of thrombosis need to be considered in the patient with suspected disease. Sometimes, the cause of DVT (especially secondary VTE) is associated with more than 1 underlying condition. In a study of immobilized, general medicine patients, risk factors that were independently associated with an increased risk for thromboembolism included presence of an acute infectious disease, aged >75 years, cancer, and history of VTE.23
The most common symptoms of DVT include swelling, pain, and discoloration in the associated extremity. A palpable cord also may be present. The location of symptoms is not always directly correlated to the location of the actual thrombosis. For example, a patient may have symptomatic involvement of the entire leg but have only an isolated DVT in the tibial vein. Another patient may have symptomatic involvement of the popliteal vein but have thrombosis in other proximal veins. These symptoms are somewhat nonspecific, and further evaluation often is needed. This is where objective assessment measures play an important role.
Complete thrombosis history, which includes the age of onset, location of prior thromboses, and inclusion of objective diagnostic studies that document the specific areas of involvement in a patient, is very important.24 Family history also should be considered. The hereditary component of DVT should not be overlooked, especially if 1 or more first-degree relatives have a history of VTE. An increased susceptibility for VTE often is present when a first-degree family member has a positive history.24
Integral to the process of diagnosis is a complete interview with the patient to assess any recent exposure to risk factors or the presence of other disease states that increase the risk of VTE. The components of the physical examination in a patient with suspected DVT are many. There may be increased edema in the associated extremity. Warmth, related to the swelling and interrupted blood flow, along with erythema, is common. The patient may or may not be able to walk, although general tenderness in the extremity is common.22 A meta-analysis showed that individual clinical symptoms of DVT are poorly predictive of actual presence of DVT when not combined with formal accepted assays; and that only a difference in calf diameters was of potential value for ruling in DVT, and only the absence of calf swelling and absence of a difference in calf diameters were of value for ruling out DVT.25
As mentioned, 2 large studies showed only a small percentage of patients will actually have DVT even though their presentation suggests its presence. In these studies, 17% and 32% of patients, respectively, had DVT.20,21 The differential diagnosis can include many factors including cellulitis, swelling because of muscle strain/tear or paralysis, lymph obstruction, Baker's cyst, and knee abnormality.26
Objective studies for diagnosis of VTE may include D-dimer testing, contrast venography, compression ultrasonography, and impedance plethysmography. These procedures can be both invasive and noninvasive. A review of the literature suggests that compression ultrasonography is the noninvasive procedure used most often for diagnosing DVT in symptomatic patients. Invasive studies (eg, venography) are used when either a noninvasive test is negative but clinical suspicion for disease is high, or when noninvasive testing is not clinically possible as the noninvasive testing may be less accurate.27
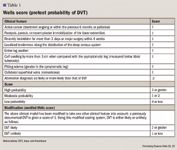
In summary, diagnosis of DVT is made up of subjective and objective measures, both having clinical relevance when ruling in or out DVT. A myriad of risk factors needs to be considered when a patient presents with classic symptoms of DVT. Objective studies may be negative for DVT; however, clinical suspicion, pre-test probability, and other subjective measures including hypercoagulable status may lead to a diagnosis of thrombosis.
ACUTE TREATMENT
The goals for acute treatment of DVT are to prevent further clotting, prevent acute pulmonary emboli, reduce the risk of recurrent thrombosis, and to truncate the development of complications including venous insufficiency and post-thrombotic syndrome. If untreated, half of all untreated individuals with acute proximal DVT will develop PE.22
Patients with acute DVT should be treated with one of several therapies. These include subcutaneous (SC) low-molecular-weight heparin (LMWH), intravenous (IV) unfractionated heparin (UFH), SC UFH with monitoring, fixed-dose SC UFH, or SC fondaparinux, versus no treatment at all.31 For patients with high clinical suspicion of DVT, anticoagulants should be employed until diagnostic testing confirms. It is now recommended that patients with acute DVT be started on a vitamin K antagonist (VKA) on treatment day 1 rather than delaying VKA therapy. Therapy with UFH, LMWH, or fondaparinux should continue for at least 5 days and until the international normalized ratio (INR) is ≥2 for 24 hours.31
Selected patients may receive catheter-directed thrombolysis. The updated 2008 American College of Chest Physicians (ACCP) guidelines discuss the use of catheter-directed thrombolysis along with both pharmacologic and nonpharmacologic measures to correct underlying venous abnormalities.31 This particular topic is not discussed in detail here, for purposes of this article.
Vena caval filters are not routinely recommended in addition to anticoagulants for the treatment of acute DVT or PE. For patients with acute proximal DVT or PE where anticoagulant therapy is not possible due to risk of bleeding, the placement of an inferior vena caval filter is recommended. For patients with proximal DVT or PE who have an inferior vena caval filter placed as an alternative to anticoagulation, it is recommended that a conventional course of anticoagulant therapy be started if the risk of bleeding resolves.31
The advent of LMWH brought with it greater bioavailability and more predictable pharmacologic effects versus UFH. For this reason, specific laboratory monitoring is not necessary for patients using LMWH. The most commonly used LMWH is enoxaparin. It is also a more convenient outpatient alternative to IV UFH. Dalteparin and tinzaparin are also alternative LMWHs for use in the outpatient setting.
The dosing of enoxaparin can be once or twice daily depending on individual patient characteristics. For DVT with or without PE, the dosage is 1 mg/kg SC every 12 hours or 1.5 mg/kg every 24 hours, for a minimum of 5 days and up to 17 days. Enoxaparin does require renal dosing adjustments for creatinine clearance <30 mL/min. In these patients, UFH is recommended over LMWH. However, if LMWH is used, the dose should be reduced by 50%, and monitoring of anti-factor Xa levels may be necessary to monitor anticoagulant effect. Inpatients and outpatients with renal insufficiency may receive 1 mg/kg every 24 hours. Monitoring for signs and symptoms of bleeding is necessary in all patients using enoxaparin, regardless of dose requirement.32
Contraindications to its use include active major bleeding; hypersensitivity to enoxaparin, heparin, or pork products; hypersensitivity to benzyl alcohol (when using multi-dose vials); and thrombocytopenia associated with a positive test for antiplatelet antibody in the presence of enoxaparin.32
Common adverse effects with use of enoxaparin include edema, diarrhea, nausea, hematoma (local), confusion, pain, dyspnea, injection site irritation, and fever. Serious adverse effects include atrial fibrillation and heart failure (<1%), eczematous drug eruption, major hemorrhage (4% or less), thrombocytopenia (<3%), increased liver function tests (6%), anaphylactoid reaction, spinal hematoma (rare), pulmonary edema, and pneumonia (<1%).32
Dalteparin is FDA-approved for use in medical patients with restricted mobility as well as in patients with postoperative DVT. Dosing in medical patients with restricted mobility is 5,000 international units (IU) SC once daily for 12 to 14 days. Contraindications to its use include hypersensitivity to dalteparin, heparin, or pork products as well as active major-bleeding, dalteparin-induced thrombocytopenia, and regional anesthesia. Precautions with its use include but are not limited to active or history of gastrointestinal (GI) ulceration or hemorrhage, bacterial endocarditis, diabetic retinopathy, hemorrhagic stroke, history of heparin-induced thrombocytopenia, and uncontrolled hypertension.33
Common adverse effects of dalteparin include injection-site hematoma (7%–35%) and injection-site pain (4.5%–12%). Serious adverse effects include intracranial hemorrhage, subdural hemorrhage, thrombocytopenia (<1% in non-cancer patients, 10.9%–13.6% in patients with cancer), increased liver function tests (up to 4.3%), and anaphylactoid reaction (rare).33
The dosing of tinzaparin for DVT is 175 IU SC once daily for at least 6 days, or until the patient is adequately anticoagulated with warfarin. It is not recommended to use tinzaparin in patients aged >90 years with a creatinine clearance of <60 mL/min. Its use is contraindicated in patients with active major bleeding, current or history of heparin-induced thrombocytopenia, or known sensitivity to tinzaparin, heparin, pork products, sulfites, or benzyl alcohol. Several precautions exist for patients with various types of recent or current hemorrhage.34
Common adverse effects of tinzaparin include erythema (16%), asymptomatic elevated liver function tests (9%–13%), injection-site pain (16%), and irritation (16%). More serious adverse effects include major bleeding (0.8%), granulocytopenic disorder (rare), spinal/epidural hematoma (rare), pancytopenia (rare), thrombocytopenia (1%), severe thrombocytopenia (0.13%), anaphylaxis (rare), priapism (rare), and death.34
A boxed warning exists for all LMWH products when used in patients receiving neuraxial anesthesia Development of spinal hematoma has been documented. Further information on this risk is included in the patient package insert.32–34 The 2008 ACCP guidelines include meta-analyses that compared the efficacy and safety of weight-based SC LMWH with both SC and IV UFH with dose adjustment.31 These meta-analyses showed that LMWH was associated with fewer thrombotic complications, less major bleeding, and fewer deaths.35,36
A common question in many anticoagulation clinics surrounds the use of once- versus twice-daily dosing of LMWH. There have been several head-to-head trials comparing the 2 dosing schemes of the same LMWH; however, the same dose of LMWH has not always been compared.37–39 Meta-analyses of several of these studies have found no difference in recurrent VTE, major bleeding, or mortality.40 Once-daily dosing of enoxaparin (1.5 mg/kg daily) is currently FDA-approved only for inpatient use. Dalteparin and tinzaparin, both once-daily medications, have been compared for outpatient use in treatment of DVT.41 No difference in recurrent VTE at 3 months, major bleeding at 7 days, or death at 3 months was found.41
A synthetic pentasaccharide. Fondaparinux is a synthetic pentasaccharide that has been used for the short-term treatment of DVT and PE. Like LMWH enoxaparin and tinzaparin, it is used in conjunction with warfarin. Dosage of fondaparinux is weight-based. For body weight <50 kg, 5 mg SC once daily is used. If body weight is 50 to 100 kg, 7.5 mg SC daily is employed. Body weight >100 kg requires 10 mg SC daily for 5 to 9 days. Treatment is continued until therapeutic INR is achieved.
Dosage in renal disease is relative to the degree of impairment. For creatinine clearance of 50 to 80 mL/min, a 25% reduction in clearance has been observed. A 40% reduction in clearance has been observed for creatinine clearance of 30 to 50 mL/min, and use of fondaparinux is contraindicated in patients with a creatinine clearance <30 mL/min. The same boxed-warning exists with use of fondaparinux in patients receiving neuraxial analgesia.42
Another contraindication to use of fondaparinux is active major bleeding, due to the risk for uncontrollable hemorrhage. Fondaparinux is also contraindicated in patients with bacterial endocarditis, body weight <50 kg (during prophylaxis), and thrombocytopenia (when positive on in vitro test for antiplatelet antibody). Precautions include but are not limited to indwelling epidural catheter, arterial hypertension, diabetic retinopathy, patients aged ≥65 years, ulcerative and angiodysplastic GI disease, and hemorrhagic stroke.42
Fondaparinux is a factor Xa inhibitor that is given subcutaneously and can be taken on an outpatient basis. This convenience, along with more direct targeting of clotting at the end of the cascade, has made it a plausible alternative to LMWH therapy in patients with DVT.
The Matisse DVT trial examined the use of fondaparinux and warfarin versus enoxaparin and warfarin in patients with DVT and/or PE. In this prospective, randomized, double-blind study, patients received either subcutaneous fondaparinux once daily (weight-based dosing) along with placebo, or subcutaneous enoxaparin twice daily (weight-based, renally adjusted dosing) along with placebo. Both study groups started VKA within 72 hours and continued the study medication for at least 5 days and until INR was >2.0. The VKA was then continued for 3 months.43
This trial included patients who presented with symptomatic DVT that was then confirmed by ultrasonography or venography. The primary efficacy end point included recurrent, symptomatic VTE within the 90-day study period, which was defined as DVT, PE, or death in which PE was contributory or could not be fully ruled out. Major bleeding during the initial treatment period and 3-month mortality were safety end points.43
The mean duration of treatment with fondaparinux and enoxaparin were equal in both groups. Of the 2,205 patients randomly assigned, recurrent VTE occurred in 3.9% of patients within the fondaparinux group and in 4.1% of patients in the enoxaparin group. Death due to PE was equal in both groups (5 patients); however, nonfatal PE occurred more often in the fondaparinux (n=20) versus enoxaparin (n=12) groups. DVT alone occurred in more patients in the enoxaparin group (n=28) than in the fondaparinux group (n=18). Major bleeding occurrences were nearly equal. In the 90-day treatment period, 41 fondaparinux patients died versus 33 in the enoxaparin group. None of the aforementioned differences were statistically significant. Thus, the authors concluded that fondaparinux is not inferior to enoxaparin in the treatment of acute, symptomatic DVT and is not associated with a higher risk of bleeding. This trial demonstrates, however, that dosing of fondaparinux based on body weight can be difficult.43
A second study examined the safety and efficacy of fondaparinux when incorporated into a VTE prevention protocol in patients that had undergone trauma, as trauma is a leading cause of thrombosis in patients. This study stratified patients by risk (high risk or very high risk). The study design assigned high-risk patients to receive fondaparinux 2.5 mg daily, while very-high-risk patients received fondaparinux 2.5 mg daily and pneumatic compression boots. If a patient was not a candidate for anticoagulation, pneumatic compression only was used. All patients received identical ultrasound studies at enrollment and 1 week later. Although a small study enrolling 87 patients, the overall incidence of DVT was 4.6%. At the study outset, it was hypothesized that the DVT rate in high-risk patients receiving fondaparinux would be <5%. There was no PE, thrombocytopenia, or attributable bleeding in the fondaparinux group. The authors concluded that fondaparinux appears to offer protection against VTE in high-risk trauma patients as well as being convenient, more cost-effective, and reducing the risk of heparin-induced thrombocytopenia.44
If using IV UFH, it is recommended that a starting dose of 80 U/kg or a 5,000 U IV bolus be given. Following this, heparin should be infused at 18 U/kg/h or 1,300 U/h, and adjusted to an activated partial thromboplastin time (aPTT) that corresponds to 0.3–0.7 IU/mL of anti-factor Xa activity. SC UFH monitored is given as 17,500 U or a weight-based adjusted dose of 250 U/kg twice daily, with dose adjusted to maintain aPTT that corresponds to that of IV UFH use. Fixed-dose SC UFH unmonitored is recommended at a dose of 333 U/kg followed by a dose of 250 U/kg twice daily.
Contraindications to the use of heparin include active bleeding, severe thrombocytopenia, and instances in which blood coagulation tests cannot be performed at appropriate intervals. Precautions to its use are many and related to the increased risk of bleeding, including but not limited to menstruation, GI ulceration, hemophilia, and hypertension. Thrombocytopenia may occur, especially with prolonged use.45
Monitoring of heparin includes the measurement of aPTT 6 hours after initiation of the infusion until stabilized and then daily at the same time of day. Complete blood count (CBC), especially hematocrit and platelet counts, should be monitored periodically during infusion. Signs and symptoms of bleeding should be assessed regularly, including stool occult blood testing. Thrombosis can occur up to several weeks after discontinuation of heparin therapy. Heparin-induced thrombocytopenia (HIT) is the most common adverse effect of heparin therapy. HIT type 1 is nonimmune-mediated and not associated with a risk of thrombosis. Its manifestations typically resolve with discontinuation of heparin therapy. However, HIT type 2, which is immune-mediated, can have an incidence of up to 5% and is associated with thrombosis and therefore presents a higher clinical risk.46 The risk of HIT type 1 or 2 increases with longer exposure to the medication and is higher with use of UFH than with LMWH.
LMWH versus UFH. In the evaluation of LMWH versus UFH for treatment of acute DVT, many studies have looked at efficacy as well as various outcome measures and safety measures that may recommend using one of these therapies over the other. A 1996 comparison of at-home LMWH versus inpatient UFH showed that LMWH can be used at home safely and effectively to treat patients with proximal DVT. The study was completed using 500 patients who were randomly assigned to either twice daily LMWH (1 mg/kg) or IV UFH. Patients receiving IV UFH had to remain in the hospital, whereas LMWH patients were able to go home. Results of the study showed that there was no statistically significant difference in recurrent thromboembolism or in major bleeding.47 The average amount of time spent in the hospital was considerably shorter for those patients who received LMWH (1.1 versus 6.5 days).47
LMWH has fallen into favor for acute treatment of VTE given its ability to be administered in the outpatient setting as a subcutaneous injection. However, the cost of these agents is substantial, leading to questions of UFH being used in this capacity. A trial was conducted to determine if UFH could be given as a fixed-dose, subcutaneous injection in acute management.48 Researchers compared fixed-dose, weight-adjusted UFH with LMWH in a randomized, open-label, noninferiority trial including 708 patients with acute VTE in Canada and New Zealand. Patients were randomly assigned to receive either UFH at an initial dose of 333 U/kg SC followed by a fixed dose of 250 U/kg SC every 12 hours, or dalteparin or enoxaparin at a dose of 100 IU/kg SC every 12 hours. Both treatments were overlapped with 3 months of warfarin therapy. Warfarin was initiated the same day as UFH or LMWH, and these interventions were continued until the INR was ≥2.0 for 48 hours. The primary outcome was recurrent VTE within 3 months and major bleeding within 10 days of enrollment.48
Of the total patients randomly assigned, 355 were assigned to the UFH (study) group and 353 to the LMWH (control) group. There was no statistical difference in VTE recurrence between the groups. In the UFH group, 3.8% of patients experienced recurrent VTE, compared with 3.4% of patients in the LMWH group. There also was no statistically significant difference in the occurrence of major bleeding between the groups (4 patients in the UFH group and 5 patients in the LMWH group). The authors concluded that outpatient subcutaneous fixed-dose UFH was as safe and effective as LMWH for the acute treatment of VTE.48
The VKA warfarin should be started on treatment day 1. Warfarin is used in conjunction with the above products to maintain adequate anticoagulation, and to prevent worsening of clotting, formation of pulmonary emboli, and recurrent clotting in the long term. It is recommended that warfarin be started at a dose of 2 to 5 mg daily and titrated to a target INR of 2.5 (range, 2–3).31,49,50 Observational studies have failed to show a benefit of starting warfarin at a dose of 10 mg daily.50,51 Typical maintenance doses range from 2 to 10 mg daily, although some patients may require <2 mg or >10 mg daily to maintain therapeutic INR. The goal INR range for a patient on warfarin for acute treatment of DVT is 2 to 3, with a target of 2.5.
Dose adjustments are made based on the INR. Along with withholding of a single dose or doses (for supratherapeutic INR) or giving additional warfarin doses (for subtherapeutic INR), weekly maintenance doses may need to be adjusted to maintain therapeutic INR. There exist cases in which lower dose initiation is necessary, for patients with cytochrome P450 2C9 (CYP2C9) and vitamin K epoxide reductase complex subunit 1 (VKORC1) genetic variations.49
Contraindications to the use of warfarin are many and include, but are not limited to, blood dyscrasias, bacterial endocarditis, malignant hypertension, inadequate laboratory facilities, pregnancy, lack of patient cooperation because of alcoholism or senility, procedures that introduce uncontrollable bleeding, and hemorrhagic tendencies. Precautions include, but are not limited to, malignancy, CYP2C9 and VKORC1 genetic variations, congestive heart failure, diarrhea, edema, hepatic impairment, and HIT.49 The list of medications that interact with warfarin is extensive. Concomitant use of these medications is not necessarily contraindicated. However, increased frequency of monitoring and dose adjustment of either warfarin or the interacting medication may be necessary to maintain therapeutic INR.
Adverse effects of therapy with warfarin include cholesterol embolus syndrome (rare), hypersensitivity (rare), hemorrhage, tissue necrosis, and intraocular hemorrhage (5%–11%).49
Monitoring the patient includes subjective and objective parameters and must be planned in cooperation between the patient and the healthcare provider. Baseline and periodic CBC is monitored as well as the INR. INR monitoring is done by individual anticoagulation clinic protocol. However, its monitoring is done more frequently at the initiation of warfarin therapy, with changes in the dose of warfarin, or with changes in the physical status of the patient. Liver function testing is often performed as well. Patients as well as providers need to monitor for the signs and symptoms of bleeding.
A boxed warning is also in effect for warfarin due to the risk of major or fatal bleeding. Due to this, regular monitoring of INR is necessary in all patients receiving the drug.49 Please refer to warfarin patient package insert for full information regarding this boxed warning.
WARFARIN DURATION OF TREATMENT
After successful initiation of warfarin and discontinuation of the chosen bridge therapy, long-term use of warfarin is recommended for continued prevention of VTE.31 Duration of therapy differs based on the indication for therapy. Short-term, intermediate, and indefinite periods of anticoagulation have been studied, and the intensity of treatment also has been considered.31 Regarding duration of treatment, the ACCP currently recommends the following intervals:
Regarding intensity of treatment, the ACCP recommends a target INR of 2.5 (range, 2.0–3.0) for treatment of DVT, for all treatment durations. In patients with unprovoked DVT who have a strong preference for less-frequent INR testing to monitor therapy, after the first 3 months of conventional-intensity anticoagulation (INR range, 2.0–3.0), low-intensity therapy (INR range, 1.5–1.9) with less frequent INR monitoring is recommended over stopping treatment. High-intensity VKA therapy (INR range, 3.1–4.0) is not recommended.31
The treatment of asymptomatic DVT of the leg is identical to that of symptomatic DVT of the leg.31
IMPORTANCE OF PROPHYLAXIS
VTE prophylaxis is critical when caring for hospitalized patients. Most inpatients have at least 1 risk factor for VTE, and close to 40% have 3 or more.52 The incidence of hospital-acquired DVT is as great as 40% in general surgery or medical patients who do not receive prophylaxis, and increases to near 60% in patients who undergo orthopedic surgeries without thromboprophylaxis.52,53 VTE increases the rates of morbidity and mortality as well as total healthcare costs. A study conducted showed that development of hospital-acquired VTE can increase length of stay by 6 days and increase mortality by approximately 7%.54 The study also showed that VTE was the second-most common medical complication seen in hospitalized patients. Pulmonary embolism also has been shown to be the most common preventable cause of death in the hospitalized patient.52,53
Long periods of immobility can lead to thrombosis formation due to venous stasis. Therefore, early and frequent walking is essential for hospitalized patients. However, often full ambulation is not possible at the beginning of a hospital stay or after surgery, and full ambulation alone does not provide full protection against VTE.52 Use of both pharmacologic and mechanical prophylaxis has been shown to decrease rates of thrombosis development.
PHARMACOLOGIC PROPHYLAXIS
Various LMWHs are used for prophylaxis of thrombus due to immobility following surgery. The following is a breakdown of FDA-approved indications.
Enoxaparin can be used for postoperative prophylaxis in hip replacement, knee replacement, and abdominal surgery, as well as prophylaxis against DVT with restricted mobility. In hip replacement, approved dosing is either 30 mg SC every 12 hours for 7 to 10 days or 40 mg SC daily for 3 weeks. In knee replacement surgery, dosing is approved at 30 mg SC twice daily for 14 days. Abdominal surgery requires a dose of 40 mg SC daily for 7 to 10 days. Finally, DVT prophylaxis in a medical patient with restricted mobility is 40 mg SC daily for up to 14 days.32
Dalteparin is used for prophylaxis in abdominal surgery, hip surgery, and in cancer patients for the prevention of VTE. Following abdominal surgery, at-risk patients receive a dose of 2,500 IU SC every 24 hours for 5 to 10 days. High-risk patients receive double that dose, or 5,000 IU SC every 24 hours for 5 to 10 days. In hip replacement surgery, the approved dosing can be based on 3 schemes. The first scheme is 2,500 IU SC for 4 to 8 hours after surgery, then 5,000 IU every 24 hours for 5 to 10 days. The second variation is 2,500 IU 2 hours before surgery and 4 to 8 hours after surgery, then 5,000 IU every 24 hours for 5 to 10 days. Finally, 5,000 IU can be given 10 to 14 hours before surgery, 4 to 8 hours after surgery, and then every 24 hours for 5 to 10 days thereafter. For VTE prevention in the patient with cancer, the first month of dalteparin therapy is given as 200 IU/kg (maximum, 18,000 IU) SC every day. During months 2 to 6 of therapy, the dose is reduced to 150 IU/kg (maximum, 18,000 IU) SC every day. Therapy with dalteparin in cancer patients for >6 months is not adequately studied.33
Tinzaparin, another LMWH, is not indicated for prophylaxis of DVT. It is only approved for use with warfarin after diagnosis of DVT.34
Fondaparinux is approved for postoperative prophylaxis of DVT in hip, knee, and abdominal surgery. The dose is 2.5 mg SC daily for 5 to 9 days. Abdominal surgery patients may continue therapy up to 10 days. In hip-fracture patients, the dose may be given for up to 24 days.42
Heparin is used as prophylaxis against PE and VTE in patients who are immobile. The dosing of heparin for these indications is 5,000 units SC every 8 to 12 hours for 7 days or until fully ambulatory, whichever is longer.45
Warfarin may be used for the prevention of VTE in patients with appropriate risk factors. The dosing of warfarin is the same as for treatment of DVT above. For patients undergoing knee or hip arthroplasty, warfarin should be given at a dosage to achieve an INR target of 2.5 (range, 2.0–3.0). Thromboprophylaxis with warfarin should continue for a minimum of 10 days. For patients undergoing hip arthroplasty or hip-fracture surgery, thromboprophylaxis should continue more than 10 days and up to 35 days.50
MECHANICAL PROPHYLAXIS
Mechanical prophylaxis is thought to prevent VTE formation by increasing venous outflow and decreasing venous stasis. Three forms of mechanical prophylaxis are currently available: graduated compression stockings, intermittent pneumatic compression devices, and venous foot pumps. Each of these modalities has various products available, differing in length, compression cycles, pressure or fit, without any accepted standard or comparative data. Additionally, mechanical thromboprophylaxis options are not required to prove efficacy in preventing VTE before being approved or marketed.52,55
The sole benefit to this group of prophylaxis agents is the lack of bleeding complications.52 While studies have proven these modalities to be efficacious in preventing DVT, there have been no adequately sampled studies conducted to show their efficacy in preventing PE or decreasing risk of death associated with VTE. Mechanical methods have also been studied less frequently than pharmacologic agents, and several studies have concluded that anticoagulant thromboprophylaxis is more efficacious.56–59 Difficulties in compliance with the mechanical options may also lead to decreased efficacy.60 As such, the 2008 ACCP guidelines recommend that mechanical prophylaxis be used as first line only in patients at high bleeding risk and only as an adjunct to anticoagulant-based thromboprophylaxis in patients with a low-to-moderate bleeding risk.52
CONCLUSION
VTE is a common medical condition caused by a myriad of risk factors, which can lead to increased morbidity, mortality, and significant healthcare costs. The correct diagnosis and acute treatment of this disease is critical. Many treatment options exist for treatment of DVT and PE, as well as for the prevention of secondary venous thromboemboli and depend upon specific patient characteristics. Clinical practice guidelines have been developed that can assist practitioners in choosing the most beneficial and cost-effective option for their patient.
Dr Wood and Dr Fitzpatrick are both clinical pharmacy specialists at the Veterans Affairs Boston Healthcare System, Mass.
Disclosure Information: The authors report no financial disclosures as related to products discussed in this article.
REFERENCES
1. Büller H, Agnelli G, Hull R, Hyers TM, Prins MH, Raskob GE. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(suppl 3):401S–428S.
2. White R. The epidemiology of venous thromboembolism. Circulation. 2003;107(suppl 1):I4–I8.
3. Silverstein M, Heit J, Mohr D, Petterson T, O'Fallon W, Melton L. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158:585–593.
4. Anderson F Jr., Spencer F. Risk factors for venous thromboembolism. Circulation. 2003;107:I9–I16.
5. Hansson P, Sörbo J, Eriksson H. Recurrent venous thromboembolism after deep vein thrombosis: incidence and risk factors. Arch Intern Med. 2000;160:769–774.
6. Heit J, Mohr D, Silverstein M, Petterson T, O'Fallon W, Melton L. Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study. Arch Intern Med. 2000;160:761–768.
7. Schulman S, Lockner D, Juhlin-Dannfelt A. The duration of oral anticoagulation after deep vein thrombosis: a randomized study. Acta Med Scand. 1985;217:547–552.
8. Lee A, Levine M. Venous thromboembolism and cancer: risks and outcomes. Circulation. 2003;107(suppl 1):I17–I21.
9. Haines S, Witt D, Nutescu E. Venous thromboembolism. In: DiPiro JT, et al. Pharmacotherapy: A Pathophysiologic Approach. 7th ed. New York, NY: McGraw-Hill, 2008:331–371.
10. Thomas R. Hypercoagulability syndromes. Arch Intern Med. 2001;161:2433–2439.
11. Rosendaal F, Helmerhorst F, Vandenbroucke J. Female hormones and thrombosis. Arterioscler Thromb Vasc Biol. 2002;22:201–210.
12. Scurr J, Machin S, Bailey-King S, Mackie U, McDonald S, Smith PD. Frequency and prevention of symptomless deep-vein thrombosis in long-haul flights; a randomised trial. Lancet. 2001;357:1485–1489.
13. Lapostolle F, Surget V, Borron S, et al. Severe pulmonary embolism associated with air travel. N Engl J Med. 2001;345:779–783.
14. Turpie A, Chin B, Lip G. Venous thromboembolism: pathophysiology, clinical features, and prevention. BMJ. 2002;325:887–890.
15. Kearon C. Natural history of venous thromboembolism. Circulation. 2003;107(suppl 1):I22–I30.
16. Dahlbäck B. Blood coagulation. Lancet. 2000;355:1627–1632.
17. Moser KM, LeMoine JR. Is embolic risk conditioned by location of deep venous thrombosis? Ann Intern Med. 1981;94:439–444.
18. Turkstra F, Kuijer PM, van Beek EJ, Brandjes DP, ten Cate JW, Büller HR. Diagnostic utility of ultrasonography of leg veins in patients suspected of having pulmonary embolism. Ann Intern Med. 1997;126:775–781.
19. Meignan M, Rosso J, Gauthier H, et al. Systematic lung scans reveal a high frequency of silent pulmonary embolism in patients with proximal deep venous thrombosis. Arch Intern Med. 2000;160:159–164.
20. Birdwell BG, Raskob GE, Whitsett TL, et al. The clinical validity of normal compression ultrasonography in outpatients suspected of having deep venous thrombosis. Ann Intern Med. 1998;128:1–7.
21. Huisman MV, Büller HR, ten Cate JW, Vreeken J. Serial impedance plethysmography for suspected deep venous thrombosis in outpatients. The Amsterdam General Practitioner Study. N Engl J Med. 1986;314:823–828.
22. Landaw SA, Bauer KA. Approach to the diagnosis and therapy of deep vein thrombosis. In: UpToDate, Leung, LLK, UpToDate, Waltham, MA, 2009.
23. Alikhan R, Cohen AT, Combe S, et al; MEDENOX Study. Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX Study. Arch Intern Med. 2004;164:963–968.
24. Bezemer ID, van der Meer FJ, Eikenboom JC, Rosendaal FR, Doggen CJ. The value of family history as a risk indicator for venous thrombosis. Arch Intern Med, 2009;169:610–615.
25. Goodacre S, Sutton AJ, Sampson FC. Meta-analysis: the value of clinical assessment in the diagnosis of deep venous thrombosis. Ann Intern Med. 2005;143:129–139.
26. Hull RD, Hirsh J, Sackett DL, et al. Clinical validity of a negative venogram in patients with clinically suspected venous thrombosis. Circulation. 1981;64:622–625.
27. Kearon C, Julian JA, Math M, Newman TE, Ginsberg JS. Noninvasive diagnosis of deep venous thrombosis. McMaster Diagnostic Imaging Guidelines. Ann Intern Med. 1998;128:663–667.
28. Pineo GF. Prevention of venous thromboembolic disease in medical patients. In: UpToDate, Leung, LLK, UpToDate, Waltham, MA, 2009.
29. Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350:1795–1798.
30. Wells PS, Anderson DR, Rodger M, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349:1227–1235.
31. Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Camerata AJ; American College of Chest Physicians. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S–545S.
32. Lovenox (enoxaparin) [package insert]. Bridgewater, NJ: Sanofi-Aventis; 2008.
33. Fragmin (dalteparin) [package insert]. Woodcliff Lake, NJ: Eisai Inc; 2008.
34. Innohep (tinzaparin) [package insert]. Ballerup, Denmark: LEO Pharma; 2009.
35. van Dongen CJ, van den Belt AG, Prins MH, Lensing AW. Fixed dose subcutaneous low-molecular-weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2004(4):CD001100.
36. Dolovich LR, Ginsberg JS, Douketis JD, Holbrook AM, Cheah G. A meta-analysis comparing low-molecular-weight heparins with unfractionated heparin in the treatment of venous thromboembolism: examining some unanswered questions regarding location of treatment, product type, and dosing frequency. Arch Intern Med. 2000;160:181–188.
37. Breddin HK, Hach-Wunderle V, Nakov R, Kakkar VV; CORTES Investigators. Effects of a low-molecular-weight heparin on thrombus regression and recurrent thromboembolism in patients with deep-vein thrombosis. N Engl J Med. 2001;344:626–631.
38. Charbonnier BA, Fiessinger JN, Banga JD, Wenzel E, d'Azemar P, Sagnard L. Comparison of a once daily with a twice daily subcutaneous low molecular weight heparin regimen in the treatment of deep vein thrombosis. FRAXODI Group. Thromb Haemost. 1998;79:897–901.
39. Holmoström M, Berglund MC, Granquist S, Bratt G, Törnebohm F, Lockner D. Fragmin once or twice daily subcutaneously in the treatment of deep venous thrombosis of the leg. Thromb Res. 1992;67:49–55.
40. Couturaud F, Julian JA, Kearon C. Low mole-cular weight heparin administered once versus twice daily in patients with venous thromboembolism: a meta-analysis. Thromb Haemost. 2001;86:980–984.
41. Wells PS, Anderson DR, Rodger MA, et al. A randomized trial comparing 2 low-molecular-weight heparins for the outpatient treatment of deep vein thrombosis and pulmonary embolism. Arch Intern Med. 2005;165:733–738.
42. Arixtra (fondaparinux) [package insert]. Research Triangle Park, NC: GlaxoSmithKline.; 2008.
43. Büller HR, Davidson BL, Decousus H, et al; Matisse Investigators. Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis: a randomized trial. Ann Intern Med. 2004;140:867–873.
44. Lu J, Knudson MM, Bir N, Kallet R, Atkinson K. Fondaparinux for prevention of venous thromboembolism in high-risk trauma patients: a pilot study. J Am Coll Surg. 2009; 209:589–594.
45. Heparin [package insert]. Cincinnati, OH: Celsus Laboratories; 2005.
46. Coutre S. Heparin-induced thrombocytopenia. In: UpToDate, Leung, LLK, UpToDate, Waltham, MA, 2009.
47. Levine M, Gent M, Hirsh J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med. 1996;334:677–681.
48. Kearon C, Ginsberg J, Julian JA, et al; Fixed-Dose Heparin (FIDO) Investigators. Comparison of fixed-dose weight-adjusted unfractionated heparin and low-molecular-weight heparin for acute treatment of venous thromboembolism. JAMA. 2006;296:935–942.
49. Coumadin (warfarin) [package insert]. Princeton, NJ: Bristol-Myers Squibb; 2007.
50. Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G; American College of Chest Physicians. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 suppl):160S–198S.
51. Garcia D, Regan S, Crowther M, Hughes RA, Hylek EM. Warfarin maintenance dosing patterns in clinical practice: implications for safer anticoagulation in the elderly population. Chest. 2005;127:2049–2056.
52. Geerts WH, Bergqvist D, Pineo GF, et al; American College of Chest Physicians. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 suppl):381S–453S.
53. Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 suppl):338S–400S.
54. Zhan C, Miller M. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290:1868–1874.
55. Best A, Williams S, Crozier A, Bhatt R, Gregg PJ, Hui AC. Graded compression stockings in elective orthopaedic surgery. An assessment of the in vivo performance of commercially available stockings in patients having hip and knee arthroplasty. J Bone Joint Surg Br. 2000;82:116–118.
56. Blanchard J, Meuwly J, Leyvraz P, et al. Prevention of deep-vein thrombosis after total knee replacement. Randomised comparison between a low-molecular-weight heparin (nadroparin) and mechanical prophylaxis with a foot-pump system. J Bone Joint Surg Br. 1999;81:654–659.
57. Freedman K, Brookenthal K, Fitzgerald R, Williams S, Lonner JH. A meta-analysis of thromboembolic prophylaxis following elective total hip arthroplasty. J Bone Joint Surg Am. 2000;82:929–938.
58. Lachiewicz P, Kelley S, Haden L. Two mechanical devices for prophylaxis of thromboembolism after total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Br. 2004;86:1137–1141.
59. Francis C, Pellegrini V Jr., Marder V, et al. Comparison of warfarin and external pneumatic compression in prevention of venous thrombosis after total hip replacement. JAMA. 1992;267:2911–2915.
60. Handoll HHG, Farrar MJ, McBirnie J, Tytherleigh-Strong GM, Milne AA, Gillespie WJ. Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database Syst Rev. 2002(4):CD000305.
Coalition promotes important acetaminophen dosing reminders
November 18th 2014It may come as a surprise that each year Americans catch approximately 1 billion colds, and the Centers for Disease Control and Prevention estimates that as many as 20% get the flu. This cold and flu season, 7 in 10 patients will reach for an over-the-counter (OTC) medicine to treat their coughs, stuffy noses, and sniffles. It’s an important time of the year to remind patients to double check their medicine labels so they don’t double up on medicines containing acetaminophen.
Support consumer access to specialty medications through value-based insurance design
June 30th 2014The driving force behind consumer cost-sharing provisions for specialty medications is the acquisition cost and not clinical value. This appears to be true for almost all public and private health plans, says a new report from researchers at the University of Michigan Center for Value-Based Insurance Design (V-BID Center) and the National Pharmaceutical Council (NPC).
Management of antipsychotic medication polypharmacy
June 13th 2013Within our healthcare-driven society, the increase in the identification and diagnosis of mental illnesses has led to a proportional increase in the prescribing of psychotropic medications. The prevalence of mental illnesses and subsequent treatment approaches may employ monotherapy as first-line treatment, but in many cases the use of combination of therapy can occur, leading to polypharmacy.1 Polypharmacy can be defined in several ways but it generally recognized as the use of multiple medications by one patient and the most common definition is the concurrent use of five more medications. The presence of polyharmacy has the potential to contribute to non-compliance, drug-drug interactions, medication errors, adverse events, or poor quality of life.
Medical innovation improves outcomes
June 12th 2013I have been diagnosed with stage 4 cancer of the pancreas, a disease that’s long been considered not just incurable, but almost impossible to treat-a recalcitrant disease that some practitioners feel has given oncology a bad name. I was told my life would be measured in weeks.
