- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Tocilizumab: A humanized anti-IL-6 receptor monoclonal antibody for the treatment of rheumatoid arthritis
Tocilizumab, an investigational agent for the treatment of moderate-to-severe rheumatoid arthritis, is a humanized anti-IL-6 receptor monoclonal antibody. Because tocilizumab contains a mouse monoclonal antibody grafted onto human immunoglobulin, the grafted antibody is less antigenic and has a longer half-life than the mouse antibody. When administered, tocilizumab inhibits IL-6 activity by competing for both the membrane-bound and soluble types of IL-6 receptors, thus eliminating IL-6 transduction into the cell.

Key Points
Abstract
Despite the numerous medications available to control the signs and symptoms and prevent the progression of rheumatoid arthritis (RA), many patients' symptoms are not adequately controlled with available therapies. Six immunomodulating agents are currently approved by FDA for the treatment of moderate-to-severe RA in patients who have an inadequate response to conventional therapies. These agents are tumor necrosis factor (TNF)-blocking agents, selective T-cell costimulation modulators, CD20 antigens, and interleukin-1 (IL-1) receptor antagonists. Tocilizumab, an investigational agent for the treatment of moderate-to-severe RA, is a humanized anti-IL-6 receptor monoclonal antibody. Because tocilizumab contains a mouse monoclonal antibody grafted onto human immunoglobulin, the grafted antibody is less antigenic and has a longer half-life than the mouse antibody. When administered, tocilizumab inhibits IL-6 activity by competing for both the membrane-bound and soluble types of IL-6 receptors, thus eliminating IL-6 transduction into the cell. Tocilizumab's dosing interval is longer than subcutaneously administered immunomodulating agents for RA and similar to that of other intravenously administered agents. Phase 3 trials have demonstrated tocilizumab's efficacy in allowing patients to achieve improvement in American College of Rheumatology (ACR) criteria and in slowing radiographic change, including patients who were refractory to anti-TNF treatment. A BLA for tocilizumab was filed in 2007; the agent is pending approval. (Formulary. 2008;43:272–279.)
Rheumatoid arthritis (RA) is a common immune-mediated inflammatory disease that is characterized by persistent symmetric, erosive synovitis with synovial cell proliferation, leading to destructive changes in bone and cartilage. Symptoms include fatigue, weakness, joint pain, and myalgias. RA can progress to extra-articular involvement including nodules, vasculitis, eye inflammation, neurologic dysfunction, and cardiopulmonary disease. Although RA can occur at any time of life, the incidence of the disease increases with age. RA is often refractory to treatment with conventional therapies, leading to progressive joint destruction, deformity, and disability.
The goal of therapy is to prevent or control joint damage, prevent loss of function, and decrease pain. Initial pharmacologic therapy typically involves anti-inflammatory agents, such as nonsteroidal anti-inflammatory agents (NSAIDs), salicylates, and selective cyclo-oxygenase 2 (COX-2) inhibitors. Although these agents can reduce joint pain and swelling to improve joint function, they do not alter the course of the disease or prevent joint destruction. To alter the course of the disease, treatment with disease-modifying antirheumatic drugs (DMARDs) is essential. The American College of Rheumatology (ACR) guidelines recommend the initiation of DMARDs within 3 months of diagnosis to prevent or delay the progression of joint destruction.1 DMARDs commonly used in the treatment of RA include methotrexate (MTX), hydroxychloroquine, sulfasalazine, and leflunomide. Less commonly used agents include azathioprine, D-penicillamine, gold, minocycline, and cyclosporine. The ACR guidelines suggest that MTX or leflunomide should be used in all patients regardless of disease duration or level of disease activity. These guidelines recommend selection of the initial DMARD based on efficacy, convenience of administration, monitoring requirements, cost, time until benefit, and severity of adverse events. They recommend the use of biologic agents, such as TNF inhibitors, only in patients with intermediate- or long-duration RA. They also recommend these agents when patients have inadequate response or moderate disease activity despite therapy with MTX.
In recent years, the development of immunomodulating agents, such as etanercept, infliximab, and rituximab, has offered new options for patients who have had an inadequate response to other DMARDs.
In 2007, Roche/Chugai filed a BLA for tocilizumab for the reduction of the signs and symptoms of moderate-to-severe RA in adults.2
CHEMISTRY AND PHARMACOLOGY
The immune system helps the body to recognize self from foreign tissues. In patients with RA, the immune system is no longer able to differentiate self and attacks the synovial and connective tissues. As part of the response to this attack, pro-inflammatory cytokines, such as interleukin-6 (IL-6), are produced and recruited to the site. IL-6, a pleiotropic cytokine, contributes to a variety of physiologic processes; it plays an active role in inflammatory responses and immunology. The overproduction of IL-6 has been implicated in the pathology of inflammatory and autoimmune disorders, including RA.3 In patients with RA, IL-6 is overexpressed in synovial tissue; concentrations are increased in both serum and synovial fluid.4 This cytokine affects the functions of neutrophils, monocytes, T cells, B cells, and osteoclasts, which are cells that are highly activated in patients with RA. IL-6 is also the major inducer of the hepatic acute phase response.4 Hepatic acute phase response is responsible for the production of C-reactive protein (CRP), fibrinogen, and serum amyloid A and for the suppression of albumin production. Hepatic acute phase response is a key feature of RA, correlated with disease activity and joint destruction.5 IL-6 is hypothesized to have a direct role in the joint destruction observed in RA by overstimulation of osteoclast activity, which results in increased bone absorption. Large amounts of IL-6 have been found in the sera and synovial fluid in affected joints; the amount of IL-6 detected may correlate with disease activity.6 These findings have led researchers to pursue approaches to disrupt IL-6 activities as a treatment option for RA and other inflammatory conditions.
Tocilizumab, previously known as MRA, is a humanized mouse anti-human IL-6 receptor antibody. To suppress the antigenicity of the mouse antibody, tocilizumab is humanized by grafting the complementarity-determining region (CDR) of the mouse monoclonal antibody (mAb BE-8) onto human immunoglobulin G (IgG). The grafted antibody is less antigenic and has a longer half-life than the mouse antibody. When administered, tocilizumab inhibits IL-6 activity by competing for both the membrane-bound and soluble types of IL-6 receptors, thus eliminating IL-6 transduction into the cell.7
PHARMACOKINETICS

CLINICAL TRIALS
Assessment tools. The ACR criteria are referred to in nearly all published studies assessing the efficacy of RA treatments. The ACR criteria measure improvement in swollen or tender joint counts and improvement in 3 out of 5 other parameters (CRP or erythrocyte sedimentation rate, patient global assessment of disease, physician global assessment of disease, pain scale, and degree of disability based on Health Assessment Questionnaire score).9 The ACR criteria are reported as ACR 20, ACR 50, and ACR 70. These are equivalent to a 20%, 50%, and 70% improvement, respectively, in swollen and tender joint counts as well as in 3 of the other 5 criteria. In clinical trials, researchers generally report the percentage of study participants who achieved a 20%, 50%, or 70% improvement.
Studies may also separately report the CRP levels. CRP, a beta-globulin, is found in the serum of individuals with certain inflammatory and degenerative disorders, including RA.10 High levels of CRP may be indicative of acute inflammation.
In Europe, the Disease Activity Score (DAS) and European League Against Rheumatism (EULAR) response score are commonly used. The DAS is statistically derived using the number of swollen and tender joints, patient assessment of disease activity, and the erythrocyte sedimentation rate.11 The DAS provides a number between 0 (no disease activity) and 10 (high disease activity). From the score, researchers can determine whether the patient has high disease activity, low disease activity, or is in remission.
The EULAR response criteria are based on the assessment of disease activity using the DAS.11 The EULAR response criteria can be used to evaluate a patient's clinical response to therapy by comparing the DAS score at 2 time points, such as before treatment and 3 months after initiation of therapy. According to these criteria, patients are classified as good responders, moderate responders, or nonresponders.
Radiographic evidence of damage can also be used to assess the efficacy of treatments for RA. The modified Total Sharp Score (TSS) can be used to evaluate disease activity in hands and feet. The modified TSS evaluates the presence of erosions at 16 joint sites in each hand and 6 joint sites in each foot. Each joint is assigned an erosion score ranging from 0 (no erosion) to 5 (severe erosion) at each site in the hands (total, 0–160 in hands) and from 0 (no erosion) to 10 (severe erosion) at each site in the feet (total, 0–120 in feet). TSS also evaluates joint space narrowing at 15 sites in each hand and 6 sites in each foot. The narrowing scores range from 0 (no narrowing) to 4 (severe narrowing) at each site, for a total score of 0 to 120 in the hands and 0 to 48 in the feet.
Dose-escalation trials. In a phase 1/2 randomized, double-blind, placebo-controlled, dose-escalation trial, 45 patients with active RA received a single intravenous (IV) injection of tocilizumab 0.1 mg/kg (n=9), 1 mg/kg (n=9), 5 mg/kg (n=9), or 10 mg/kg (n=7) or placebo (n=11).12 The primary efficacy end point was defined as meeting the ACR 20 response criteria at Week 2 after treatment. At Week 2, a significant difference was observed between the tocilizumab 5-mg/kg group and the placebo group (percentage of tocilizumab-treated patients achieving ACR 20, 55.6%; percentage of placebo-treated patients achieving ACR 20, 0; P=.023). No statistically significant difference in ACR 20 response was observed between the other 3 tocilizumab groups and the placebo group. The mean DAS at Week 2 in patients who received tocilizumab 5 and 10 mg/kg was 4.8 (P<.001 vs placebo) and 4.7 (P<.001 vs placebo), respectively. The erythrocyte sedimentation rate and CRP values decreased significantly in the tocilizumab 5- and 10-mg/kg groups and normalized 2 weeks after treatment.
In the phase 1/2 dose-escalation study that analyzed the pharmacokinetic profile of tocilizumab, efficacy was also assessed.8 In this trial, 15 patients received IV tocilizumab 2 mg/kg (n=5), 4 mg/kg (n=5), or 8 mg/kg (n=5) biweekly for 6 weeks. Patients who demonstrated improvement in CRP or erythrocyte sedimentation rate and who tolerated tocilizumab were allowed to continue treatment for ≤24 weeks. No statistically significant difference in efficacy was noted among the 3 dose groups. Nine patients (60%) achieved ACR 20 at 6 weeks. At 24 weeks, 13 patients (87%) achieved ACR 20, 5 (33%) achieved ACR 50, and 2 (13%) achieved ACR 70. In 12 patients (80%), CRP values, erythrocyte sedimentation rate, and serum amyloid A values were completely normalized at 6 weeks.

Recently a 3-year open-label extension of the SAMURAI study confirmed tocilizumab's ability to prevent joint destruction.15 Radiographic analysis was performed on 212 patients originally enrolled in the SAMURAI study. Patients receiving tocilizumab had a lower yearly progression rate (TSS, 1.25) in the 2 years following the study compared with the progression rate during the first year (TSS, 4.93). Yearly progression rate of the DMARDs plus tocilizumab group was also reduced (TSS, 2.47) compared with the first year (TSS, 11.38).

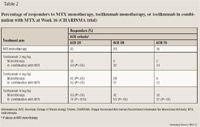
The recently published Tocilizumab Pivotal Trial in Methotrexate Inadequate Responders (OPTION), a double-blind, randomized, placebo-controlled, parallel-group study involving 623 patients with moderate-to-severe active RA, randomized patients to receive IV tocilizumab 8 mg/kg (n=205), tocilizumab 4 mg/kg (n=214), or placebo (n=204) every 4 weeks with MTX at stable prestudy doses.4 The primary end point was the proportion of patients who achieved ACR 20 at Week 24. Secondary end points included the proportion of patients who achieved ACR 50 and ACR 70 at Week 24, change from baseline in DAS at Week 24, and the proportion of patients in DAS remission at Week 24. The achievement of ACR 20 was noted in 102 patients (48%) who received tocilizumab 4 mg/kg, 120 patients (59%) who received tocilizumab 8 mg/kg, and 54 patients (26%) who received placebo (P<.0001 for both). Achievement of ACR 50 was observed in 67 patients (31%) treated with tocilizumab 4 mg/kg and 90 patients (44%) treated with tocilizumab 8 mg/kg (P<.0001 vs placebo for both). Achievement of ACR 70 was observed in 12% and 22% of patients treated with tocilizumab 4 or 8 mg/kg, respectively (P<.0001 vs placebo for both). Remission, defined as DAS28 <2.6 at 24 weeks, was achieved in 13% of patients treated with tocilizumab 4 mg/kg (P=.0002) and 27% of patients treated with tocilizumab 8 mg/kg (P<.0001) compared with 0.8% of patients who received placebo.
The Rheumatoid Arthritis Study in Anti-TNF Failures (RADIATE) evaluated the safety and efficacy of tocilizumab in patients whose RA was refractory to TNF-antagonist therapy.17 Patients (N=499) were randomized to receive IV tocilizumab 8 or 4 mg/kg or placebo every 4 weeks with stable MTX for 24 weeks. ACR 20 was achieved at 24 weeks by 50% of patients in the tocilizumab 8-mg/kg group, 30.4% of patients in the 4-mg/kg group, and 10.1% of patients in the placebo group (P<.0001 vs placebo for both). DAS28 remission at Week 24 was achieved by 30.1% of patients in the 8-mg/kg group but only 7.6% of patients in the 4-mg/kg group and 1.6% of patients in the placebo group (P=.0001 for 8 mg/kg vs placebo; P=.053 for 4 mg/kg vs placebo).

ADVERSE EVENTS
In a phase 1 trial, the most commonly reported adverse event was diarrhea, which occurred in 8% of patients.12 More than 75% of patients reported an adverse event in this trial, although no difference in the incidence or type of adverse events was observed among treatment groups receiving tocilizumab 0.1-, 1-, 5-, or 10 mg/kg. The majority of adverse events were of mild or moderate intensity.
A second phase 1 trial demonstrated that tocilizumab was well tolerated, with no severe adverse events reported.8 Increased total serum cholesterol was observed in 66% of patients. No new antinuclear antibodies or anti-DNA antibodies were observed, and no antitocilizumab antibody was detected. Two patients demonstrated decreased leukocyte counts below the normal range; 1 patient had a transient grade 3 neutropenia 1 day after the tocilizumab infusion. There were 13 adverse events related to skin and subcutaneous tissue disorders, such as dermatitis, but no injection-site reactions were reported. Common cold symptoms were reported in 33% of patients.
In the CHARISMA and OPTION investigations, nearly 50% of patients (~70% in OPTION) experienced ≥1 adverse event.4,13 The most significant adverse event in both studies was the rate of infection. In the CHARISMA study, 2.3% of patients (7/310) treated with tocilizumab experienced serious treatment-emergent infections; in the OPTION study, an infection or infestation occurred in 31% and 32% of patients receiving tocilizumab 4 or 8 mg/kg, respectively.4,13 In the OPTION trial, the most common infectious process was respiratory in nature. Other adverse events from these studies included a variety of gastrointestinal events, aggravation of RA, rash, erythema, and headache.
In the CHARISMA study, all patients who received tocilizumab had an increase in both mean alanine transaminase (ALT) and aspartate aminotransferase (AST) levels, which flowed in a sawtooth pattern between infusions.13 This increase in liver function tests was tocilizumab-related; however, in patients receiving concurrent MTX, there was an accentuated increase in ALT and AST. During the study, the greatest increase in ALT from baseline was 45% at Week 2 in patients who received tocilizumab 8 mg/kg. A total of 127 patients treated with tocilizumab experienced an ALT level greater than the upper limit of normal during the study. All patients returned to near-baseline values within 8 weeks after patients received the final dose of tocilizumab.
In the CHARISMA study, mean total bilirubin values increased continuously during the study period in the tocilizumab treatment group.13 From baseline, total bilirubin levels increased 83% by Week 16 in patients treated with tocilizumab 8 mg/kg, whereas patients treated with tocilizumab 4 mg/kg plus MTX experienced an increase of 59% by Week 14. The investigators noted that there was no relationship between the increase in ALT and elevated bilirubin; no patients experienced an increase in both ALT and bilirubin simultaneously. Elevated levels of bilirubin had generally returned to normal at follow-up.
In the tocilizumab treatment groups of the CHARISMA study, patients experienced a moderate but reversible increase in levels of mean nonfasting total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides.13 Stabilization of this increase occurred in the treatment groups, whereas the atherogenic index remained relatively unchanged. It is important to note that the atherogenic index among patients treated with tocilizumab 8 mg/kg was reduced to a level lower than its initial value at the 20-week follow-up.
In the CHARISMA study, neutrophil counts followed a dose-dependent reduction after tocilizumab administration.13 The greatest degree of neutrophil count reduction was observed at Week 14 among patients treated with tocilizumab 8 mg/kg alone or in combination with MTX (47% and 43%, respectively). The lowest neutrophil count during the study was 0.88X09/L at Week 8 in patients who received tocilizumab 8 mg/kg. The investigators reported that the neutrophil count had returned to within normal range by the follow-up visit in all but 1 patient.
Similar laboratory changes in hepatic aminotransferases, increases in serum lipid concentration, and decreases in neutrophil count also occurred in the OPTION study.4 Approximately 8% of patients who received tocilizumab experienced elevated ALT >3 times the upper limits of normal. Among patients in the tocilizumab treatment groups, 2.4% experienced ALT concentrations >5 times the upper limit of normal.
Compared with placebo, mean plasma concentrations of total cholesterol, HDL cholesterol, and low-density lipoprotein (LDL) cholesterol were increased from baseline in the tocilizumab treatment groups by Week 6 of treatment.4 Levels remained elevated for 24 weeks in the 2 treatment groups. As with the CHARISMA study, there was no increase in cardiovascular events during the 24 weeks of the OPTION study.
Administration of tocilizumab often resulted in neutrophil counts below the lower limit of normal. The rates of neutrophil decrease in the tocilizumab 4-and 8-mg/kg treatment groups were 17.4% and 32.5%, respectively. The authors determined that there was no correlation between neutropenia (<1X09 cells/L) and the occurrence or severity of infection.
DRUG INTERACTIONS
Currently, there are limited published data regarding drug interactions with tocilizumab. Various studies have evaluated tocilizumab in combination with MTX, but these studies did not report alterations in pharmacokinetics or an increased incidence of adverse effects.4,13
DOSING AND ADMINISTRATION
Tocilizumab is not yet approved by FDA; however, based on phase 2 and phase 3 investigational trials, tocilizumab is efficacious in inducing a clinical response and/or remission when it is administered at doses of 4 or 8 mg/kg via IV every 4 weeks.4 In the CHARISMA investigation, tocilizumab 8 mg/kg every 4 weeks plus MTX once weekly was demonstrated to be beneficial.13
In each issue, the "Focus on" feature reviews a newly approved or investigational drug of interest to pharmacy and therapeutics committee members. The column is coordinated by Robert A. Quercia, MS, RPh, clinical manager and director of Drug Information, Department of Pharmacy Services, Hartford Hospital, Hartford, Conn, and adjunct associate professor, University of Connecticut School of Pharmacy, Storrs, Conn; and by Craig I. Coleman, PharmD, assistant professor of pharmacy practice, University of Connecticut School of Pharmacy, and director, Pharmacoeconomics and Outcomes Studies Group, Hartford Hospital.
EDITORS' NOTE: The clinical information provided in "Focus on" articles is as current as possible. Due to regularly emerging data on developmental or newly approved drug therapies, articles include information published or presented and available to the author up until the time of the manuscript submission.
Dr Schlesselman is an assistant clinical professor, University of Connecticut School of Pharmacy, Storrs. Dr Hussey is a PGY1 resident, UMass Memorial Medical Center, Worcester.
Disclosure Information: The authors report no financial disclosures as related to products discussed in this article.
REFERENCES
1. American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002;46:328–346.
2. Roche submits application for FDA approval of Actemra for the treatment of rheumatoid arthritis [press release]. Basel, Switzerland: Roche; November 21, 2007.
3. Hirano T, Matsuda T, Turner M, et al. Excessive production of interleukin 6/B cell stimulatory factor-2 in rheumatoid arthritis. Eur J Immunol. 1988;18:1797–1801.
4. Smolen JS, Beaulieu A, Rubbert-Roth A, et al; OPTION Investigators. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): A double-blind, placebo-controlled, randomised trial. Lancet. 2008;371:987–997.
5. van Leeuwen MA, van der Heijde DM, van Rijswijk MH, et al. Interrelationship of outcome measures and process variables in early rheumatoid arthritis. A comparison of radiologic damage, physical disability, joint counts, and acute phase reactants.
6. Nakahara H, Nishimoto N. Anti-interleukin-6 receptor antibody therapy in rheumatic diseases. Endocr Metab Immune Disord Drug Targets. 2006;6:373–381.
7. Kavanaugh A. Interleukin-6 inhibition and clinical efficacy in rheumatoid arthritis treatment: Data from randomized clinical trials. Bull NYU Hosp Jt Dis. 2007;65(suppl 1):S16–20.
8. Nishimoto N, Yoshizaki K, Maeda K, et al. Toxicity, pharmacokinetics, and dose-finding study of repetitive treatment with the humanized anti-interleukin 6 receptor antibody MRA in rheumatoid arthritis. Phase I/II clinical study. J Rheumatol. 2003;30:1426–1435.
9. American College of Rheumatology Committee to Reevaluate Improvement Criteria. A proposed revision to the ACR20: The hybrid measure of American College of Rheumatology response [erratum in Arthritis Rheum. 2007;57:1574]. Arthritis Rheum. 2007;57:193–202.
10. Pinals RS, Masi AT, Larsen RA. Preliminary criteria for clinical remission in rheumatoid arthritis. Arthritis Rheum. 1981;24:1308–1315.
11. van Gestel AM, Anderson JJ, van Riel PL, et al. ACR and EULAR improvement criteria have comparable validity in rheumatoid arthritis trials. American College of Rheumatology; European League of Associations for Rheumatology. J Rheumatol. 1999;26:705–711.
12. Choy EH, Isenberg DA, Garrood T, et al. Therapeutic benefit of blocking interleukin-6 activity with an anti-interleukin-6 receptor monoclonal antibody in rheumatoid arthritis: A randomized, double-blind, placebo-controlled, dose-escalation trial. Arthritis Rheum. 2002;46:3143–3150.
13. Maini RN, Taylor RC, Szechinski J, et al; CHARISMA Study Group. Double-blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate [erratum in Arthritis Rheum. 2008;58:887]. Arthritis Rheum. 2006;54:2817–2829.
14. Nishimoto N, Hashimoto J, Miyasaka N, et al. Study of active controlled monotherapy used for rheumatoid arthritis, an IL-6 inhibitor (SAMURAI): Evidence of clinical and radiographic benefit from an x ray reader-blinded randomized controlled trial of tocilizumab. Ann Rheum Dis. 2007;66:1162–1167.
15. Nishimoto N, Hashimoto J, Miyasak N, et al. Three-year extension of the SAMURAI study confirms tocilizumab to prevent joint destruction in patients with rheumatoid arthritis. Ann Rheum Dis. 2008;67(suppl 2):335.
16. Nishimoto N, Yoshizaki K, Miyasaka N, et al. Treatment of rheumatoid arthritis with humanized anti-interleukin-6 receptor antibody: A multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 2004;50:1761–1769.
17. Emery P, Keystone E, Tony HP, et al. IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-TNF biologics: Results from a 24-week multicentre randomised placebo controlled trial. Ann Rheum Dis. 2008 [Epub ahead of print].
18. Jones G, Gu JR, Lowenstein M, et al. Tocilizumab monotherapy is superior to methotrexate monotherapy in reducing disease activity in patients with rheumatoid arthritis: The AMBITION study. Ann Rheum Dis. 2008;67(suppl 2):89.
