- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Venlafaxine associated with increased risk of suicide and attempted suicide
A large retrospective cohort study demonstrated an increased risk of suicide with use of the antidepressant venlafaxine.

Key Points
Use of the antidepressant venlafaxine is associated with greater risk of both completed and attempted suicide compared with other antidepressants, according to a large retrospective cohort study reported in the British Medical Journal (BMJ).
Previous meta-analyses of randomized, controlled clinical trials of selective serotonin reuptake inhibitors demonstrated an increased risk of worsening depression and suicidal ideation and behavior among patients aged <19 years; these analyses led to warnings from regulatory agencies in both the United States and Europe that patients using these agents should be closely monitored.
Meta-analyses have not established an association between adult use of antidepressants and increased risk of suicide, nor have observational studies established an association between venlafaxine and increased suicide risk. However, in a recent observational study, patients who were treated with venlafaxine exhibited more suicide risk factors including a previous suicide attempt, hospital admission for depression, and diagnosis of schizophrenia and bipolar disorder compared with patients who were treated with serotonin-reuptake inhibitors.
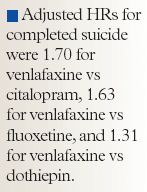
The adjusted HRs for completed suicide were 1.70 for venlafaxine versus citalopram, 1.63 for venlafaxine versus fluoxetine, and 1.31 for venlafaxine versus dothiepin. The HRs for attempted suicide were 1.20, 1.28, and 1.47, respectively.
Patients prescribed venlafaxine were twice as likely to have an overlapping prescription for another antidepressant, indicating frequent switching, possibly due to failure of the agent to achieve effect. These patients demonstrated more suicide risk factors and markers of severe and difficult-to-treat depression and psychiatric comorbidities, and they were more likely to have had previous treatment with psychotropic agents. In addition, hospital psychiatric admission and specialist care, family psychiatric history, and a history of suicide attempts were more prevalent in this population.
The authors stated that these results could indicate a causal relationship between venlafaxine use and completed or attempted suicide, because patients with more severe and treatment-resistant depression tended to be prescribed venlafaxine; however, adjustment for the measured risk factors may have left residual confounding that could explain some or all of the excess risk observed.
SOURCE
Rubino A, Roskell N, Tennis P, Mines D, Weich S, Andrews E. Risk of suicide during treatment with venlafaxine, citalolpram, fluoxetine, and dothiepin: retrospective cohort study. BMJ. 2007;334:242–245.
Employers Face Barriers With Adopting Biosimilars
March 1st 2022Despite the promise of savings billions of dollars in the United States, adoption of biosimilars has been slow. A roundtable discussion among employers highlighted some of the barriers, including formulary design and drug pricing and rebates.
