- Safety & Recalls
- Regulatory Updates
- Drug Coverage
- COPD
- Cardiovascular
- Obstetrics-Gynecology & Women's Health
- Ophthalmology
- Clinical Pharmacology
- Pediatrics
- Urology
- Pharmacy
- Idiopathic Pulmonary Fibrosis
- Diabetes and Endocrinology
- Allergy, Immunology, and ENT
- Musculoskeletal/Rheumatology
- Respiratory
- Psychiatry and Behavioral Health
- Dermatology
- Oncology
Vildagliptin: A dipeptidyl peptidase-IV inhibitor for the treatment of type 2 diabetes
Despite the variety of medications available to treat type 2 diabetes, the disease is inadequately controlled in many patients. In order to improve glycemic control, manufacturers are pursuing compounds that affect the incretin hormones that stimulate insulin release in response to increased glucose levels. Although stimulation of the incretin receptors by the glucagon-like peptide-1 (GLP-1) enhances the body's ability to produce insulin in response to elevated blood glucose concentrations, the clinical usefulness of GLP-1 is limited by its rapid degradation by dipeptidyl peptidase-IV (DPP-IV). Drug companies have developed compounds intended to act as inhibitors of DPP-IV. Vildagliptin (Galvus, Novartis) is the second DPP-IV inhibitor under investigation by FDA to offer this new mechanism to achieve glycemic control. An NDA for vildagliptin was submitted to FDA in March 2006, 1 month after the submission of the first DPP-IV inhibitor, sitagliptin.
Abstract
Despite the variety of medications available to treat type 2 diabetes, the disease is inadequately controlled in many patients. In order to improve glycemic control, manufacturers are pursuing compounds that affect the incretin hormones that stimulate insulin release in response to increased glucose levels. Although stimulation of the incretin receptors by the glucagon-like peptide-1 (GLP-1) enhances the body's ability to produce insulin in response to elevated blood glucose concentrations, the clinical usefulness of GLP-1 is limited by its rapid degradation by dipeptidyl peptidase-IV (DPP-IV). Drug companies have developed compounds intended to act as inhibitors of DPP-IV. Vildagliptin (Galvus, Novartis) is the second DPP-IV inhibitor under investigation by FDA to offer this new mechanism to achieve glycemic control. An NDA for vildagliptin was submitted to FDA in March 2006, 1 month after the submission of the first DPP-IV inhibitor, sitagliptin. Currently available clinical studies have demonstrated improved glycemic control with vildagliptin therapy in patients who have not achieved target glucose levels with diet and oral medications. (Formulary. 2006;41:494–500.)
The prevalence of type 2 diabetes is increasing worldwide. An estimated 20.8 million people have diabetes in the United States.1 Early results from the 2005 National Health Interview survey report an increase in the prevalence of diagnosed diabetes in US adults aged 18 years and older from 5.1% in 1997 to 7.4% in 2005.2 The prevalence likewise increases with age, with 17% of adults aged 65 years and older reporting a diagnosis of diabetes.3 It is predicted that more than 300 million adults will be diagnosed worldwide by 2025.1
To reduce the risk of complications, the American Diabetes Association (ADA) generally recommends a hemoglobin A1c (HbA1c) goal for patients of <7%; however, the ADA states that the ideal goal for the individual patient is an HbA1c as close to normal (<6%) as possible without significant hypoglycemia.4 Despite the benefits of lower HbA1c values, studies show that these goals are not being achieved in many patients.5
To control blood glucose, lifestyle modifications serve as the initial treatment. However, pharmacologic treatment is required if lifestyle modifications are insufficient. Typically, patients requiring pharmacologic therapy are started on an oral agent first. Fifty-three percent of adults diagnosed with diabetes report taking oral medications to control blood glucose.2 The oral medications currently available in the United States work by a variety of mechanisms, including increasing insulin action (thiazolidinediones), directly stimulating insulin secretion through closure of ATP-regulated beta cell potassium channels (sulfonylureas, repaglinide, and nateglinide), inhibiting glucose production in the liver through phosphorylation of AMP-activated protein kinase (biguanide), or reducing the influx of glucose from the gut following meal intake (alpha-glucosidase inhibitors). If blood glucose levels and HbA1c remain uncontrolled despite therapy, another oral agent or an injectable agent, such an insulin, synthetic amylin analog, or glucagon-like peptide-1 (GLP-1), can be added to therapy.
The newest agents available to treat type 2 diabetes are known as dipeptidyl peptidase-IV (DPP-IV) inhibitors. These agents alter incretin hormones, in particular preventing the degradation of GLP-1. Vildagliptin (Galvus, Novartis) is the second agent in this new class to undergo FDA review. This medication is initially being investigated to improve glycemic control in patients with type 2 diabetes who are not receiving insulin and are not achieving target glucose levels utilizing lifestyle modifications and oral medications. The manufacturer submitted an NDA for vildagliptin to FDA in March 2006.
CHEMISTRY AND PHARMACOLOGY
Vildagliptin is an orally active, potent, and selective inhibitor of DPP-IV. It is a slow-binding inhibitor with a 2-step mechanism of action that is reversible and competitive. Vildagliptin enhances levels of active GLP-1, thereby facilitating glucose-dependent insulin secretion.
Structurally, vildagliptin can be described as 1-([(3-hydroxy-1-adamantyl) amino]acetyl)-2-cyano-[S]-pyrrolidine. The adamantyl group adjacent to the amine is essential for its biological activity by providing steric bulk to the compound.6 It has a molecular weight of 303.41 g.
Following a meal, gut incretin hormones are released. The most important incretin hormones are GLP-1 and glucose-dependent insulinotropic polypeptide (GIP). These hormones, secreted in the human small intestine, are responsible for insulin release due to increased glucose levels. In contrast to agents that promote insulin secretion via glucose-independent mechanisms, GLP-1's dependence on glucose concentration is considered beneficial due to a lower risk of hypoglycemia. GLP-1 also inhibits glucagon secretion and increases beta cell mass by stimulating proliferation and neogenesis. However, the clinical utility of GLP-1 is limited by its short half-life (2 minutes). GLP-1 is rapidly degraded by the proteolytic enzyme DPP-IV.
To enhance GLP-1 activity, inhibition of the DPP-IV enzyme is emerging as a novel therapeutic approach in the treatment of diabetes. Administration of vildagliptin enhances GLP-1's ability to produce insulin in response to elevated concentrations of blood glucose, inhibit the release of glucagon following meals, slow the rate of nutrient absorption into the bloodstream, slow the rate of gastric emptying, and reduce food intake.
In a head-to-head comparison of vildagliptin with exendin-4, the agents' ability to promote islet neogenesis in mice was evaluated.8 To compare the agents, mice were dosed with vildagliptin 30 mg/kg/d orally or exendin-4 0.42 mg/kg intraperitoneal, starting 5 days prior to streptozotocin-induced beta cell injury. Vildagliptin and exendin-4 were administered daily until Day 15. Both agents decreased fasting blood glucose and glucose-AUC with sustained glucose tolerance 10 days after the last dose. Mice in both groups increased pancreatic PDX-1 mRNA levels and decreased BrdU, suggestive of enhanced differentiation of pancreatic progenitor cells.
PHARMACOKINETICS
The pharmacokinetic profile of vildagliptin in cynomolgus monkeys demonstrated that vildagliptin is rapidly absorbed following oral administration.9 Vildagliptin demonstrates an oral bioavailability of >90%. The plasma clearance rate is 1.3–1.4 L/kg. The volume of distribution (0.7 L/kg) suggests distribution to all body fluids. The elimination half-life is approximately 90 minutes. In humans >90% of DPP-IV inhibition persists for more than 12 hours following administration of a 100-mg dose.10
In a study conducted to evaluate the influence of hepatic insufficiency on vildagliptin pharmacokinetics, AUC was increased by 30% in patients with severe hepatic insufficiency.11 Exposure to inactive metabolites increased with increasing severity of impairment. The elimination half-life was unchanged by hepatic insufficiency.
CLINICAL TRIALS
In a randomized, double-blind, placebo-controlled trial, researchers evaluated 16 patients with type 2 diabetes.12 On separate days, patients received 100 mg vildagliptin or placebo followed by a 6-hour meal tolerance test to assess hepatic and peripheral glucose metabolism. Following vildagliptin administration, suppression of endogenous glucose production was greater than with placebo (1.02±0.06 versus 0.74±0.06 mg/kgmin, P=.004). With vildagliptin, the insulin secretion rate increased by 21% (P=.003 vs placebo), whereas the suppression of mean plasma glucagons was 93% greater (P<.01).
Improved metabolic control was observed with vildagliptin in patients with diet-controlled diabetes.10 In this 4-week, randomized, placebo-controlled trial with vildagliptin 100 mg, the improved control was associated with reduced glucagon levels in response to a meal. The glucagon response was reduced by vildagliptin from 88±8 pg/mL to 77±5 pg/mL (P=.001). In contrast, post-meal insulin levels were not altered by vildagliptin therapy.
Pratley and Galbreath14 also performed a 12-week placebo-controlled study of vildagliptin in treatment-naïve patients with type 2 diabetes. Patients receiving 25 mg twice daily exhibited a reduction in fasting plasma glucose of 1.1±0.4 (P=.0043) and in 4-hour mean postprandial glucose of 1.9±0.5 mM (P<.0001). Vildagliptin patients exhibited an adjusted mean change in HbA1c of –0.6±0.1% (P=.0012 vs placebo). In patients with a baseline HbA1c between 8.0% and 9.5%, the difference in HbA1c was 1.2% relative to placebo. In patients with a baseline HbA1c between 7% and 8%, the difference in HbA1c was 0.7%. Forty-seven percent of patients taking vildagliptin with a baseline HbA1c >7% reached an end point HbA1c <7%.
Although glucagon levels only increase in response to a meal, Kelley et al15 evaluated whether vildagliptin increases GLP-1 and GIP levels in the absence of a meal stimulus. The 4-week study involved 11 insulin pump-treated patients with type 1 diabetes and 9 drug-naïve patients with type 2 diabetes. Prior to treatment with vildagliptin 100 mg twice daily, GLP-1 levels were undetectable in 5 of the patients with type 2 diabetes and 9 of the patients with type 1 diabetes. After 4 weeks, GIP was increased by more than 2-fold in patients with type 1 and type 2 diabetes (P=.021 for type 1 and P=.049 for type 2). Active GLP-1 was increased by more than 9 pM in patients with type 1 diabetes (P<.001) and by more than 14 pM in patients with type 2 diabetes (P=.004).
Another study evaluated the effect of vildagliptin on acute insulin response to glucose and insulin sensitivity.16 Drug-naïve patients with type 2 diabetes were given vildagliptin 50 mg twice daily or placebo for 12 weeks followed by 2- to 4-week washout periods. During the study, acute insulin response and insulin sensitivity were determined during intravenous glucose tolerance tests. Intact GLP-1 levels were not significantly increased. Patients receiving vildagliptin exhibited increased acute insulin response to glucose from 16±7 pM to 54±9 pM (P<.001). Insulin sensitivity also increased from 1.4±0.3 to 2.2±0.5 L/mU/min (P=.016).
Matikainen et al17 evaluated the effects of vildagliptin 50 mg twice daily on postprandial lipid and lipoprotein metabolism in drug-naïve patients with type 2 diabetes. In this 4-week, randomized, double-blind placebo-controlled study, triglyceride, cholesterol, lipoprotein, glucose, insulin, glucagon, and GLP-1 responses to a fat-rich meal were measured for 8 hours postprandially. Vildagliptin therapy produced a significant reduction in total triglyceride AUC by 22±11% (P=.037), chylomicron triglyceride AUC by 65±19% (P=.001), chylomicron apolipoprotein B-48 AUC (P=.0037), and chylomicron cholesterol AUC (P=.046). As with other studies, vildagliptin therapy increased GLP-1 while decreasing glucagon secretion, glucose, and HbA1c (P<.001).
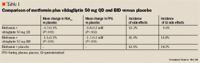
A 12-week, multicenter, randomized, double-blind, placebo-controlled trial conducted by Ahren et al20 compared the effects of treatment with vildagliptin in 107 patients with type 2 diabetes continuing a stable dosage of metformin (1,500–3,000 mg/d). The 12-week study was followed by a 40-week extension in 71 patients. At 12 weeks, the vildagliptin plus metformin group demonstrated a decrease in HbA1c of –0.6±0.1% compared with the placebo plus metformin group, which did not change (P<.0001). Fasting plasma glucose was reduced by 1.2±0.4 mmol/L (P=.0057) in the vildagliptin group, and the mean prandial glucose was reduced by 2.2±0.4 mmol/L (P<.0001). At the end of 52 weeks, between-group differences in change in HbA1c, fasting plasma glucose, and mean prandial glucose were –1.1±0.2% (P<.0001), –1.1±0.5mmol/L (P=.0312), and –2.4±0.6 mmol/L (P=.0001), respectively.
In another study by Ahren et al21 utilizing data from the previous 12-week study with a 40-week extension, the investigators evaluated vildagliptin's effect on meal-related beta cell function and insulin sensitivity. They observed insulin secretion was enhanced in patients receiving vildagliptin plus metformin but reduced in patients receiving placebo plus metformin. The group difference was reported as 0.011±0.03 pmol/L 30 min/mmol/L (P=.018). The insulin sensitivity during meal ingestion increased in the vildagliptin group but was unaltered in the placebo group (P=.036).
Rosenstock et al22 conducted a 24-week, multicenter, randomized, double-blind study comparing the efficacy and tolerability of vildagliptin 50 mg twice daily (n=459) with that of rosiglitazone 8 mg daily (n=238). The adjusted mean change in HbA1c in vildagliptin-treated patients was –1.1±0.1% from baseline. Non-inferiority to rosiglitazone was established. Compared with rosiglitazone, vildagliptin improved lipid profiles, as demonstrated by decreased total cholesterol (–14%, P<.001), LDL (–16%, P<.001), triglycerides (–9%, P=.010), non-HDL (–16%, P<.001), and VLDL (-8%, P=.007); however, only a small increase was observed in HDL (–5%, P=.003). Body weight was not affected by vildagliptin, with an adjusted mean change of 0.3±0.2 kg compared with an adjusted mean body weight change of 1.6±0.3 kg with rosiglitazone (P<.001 versus vildagliptin). The incidence of side effects was 61.4% with vildagliptin versus 64% with rosiglitazone.
A smaller study (n=12) evaluated the safety, tolerability, and therapeutic value of vildagliptin in combination with pioglitazone.23 Patients were maintained on pioglitazone 45 mg daily for 8 weeks, then randomized to receive placebo or vildagliptin 100 mg daily in combination with pioglitazone for 28 days. For the final 7 days, patients were maintained on vildagliptin alone. Peak plasma concentrations were unchanged for either medication when administered alone and in combination. Active GLP-1 levels were increased following 28 days of combination therapy compared with pioglitazone alone. Post-prandial glucose levels were also reduced by 10% following coadministration.
ADVERSE EVENTS
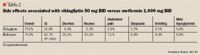
In studies, vildagliptin was generally well tolerated. Reported adverse effects were mild-to-moderate, with the most common adverse events reported being headache (7.1%), abdominal pain (4.3%), dizziness (8.6%),25 increased blood pressure (5.7%), increased sweating (5.7%), and nausea (3.8%).26 In dose response studies, no severe cases of hypoglycemia were reported and no patients discontinued therapy due to hypoglycemia.26

DRUG INTERACTIONS
Limited published information exists documenting drug interactions with vildagliptin. In studies, no statistically or clinically significant pharmacokinetic interactions occurred with glyburide26 or pioglitazone.24 In a 24-week study, patients receiving vildagliptin in combination with metformin exhibited an increased incidence of gastrointestinal side effects.
DOSING AND ADMINISTRATION
Vildagliptin was still undergoing FDA review at the time of publication. Based on clinical trials, however, oral vildagliptin 50 mg once or twice daily was effective in reducing HbA1c levels compared with placebo.27 Dosages up to 100 mg daily were found to be safe and well tolerated.
Dr Schlesselman is assistant clinical professor of pharmacy practice, University of Connecticut School of Pharmacy, Storrs, Conn. She can be reached at lauren.schlesselman@uconn.edu
Disclosure Information: The authors report no financial disclosures as related to products discussed in this article.
REFERENCES
1. American Diabetes Association. National Diabetes Fact Sheet 2005. Available at: http:// http://www.diabetes.org/uedocuments/NationalDiabetesFact-sheetRev.pdf. Accessed September 19, 2006.
2. Center for Disease Control and Prevention. Early release of selected estimates based on data from the January-September 2005 National Health Interview Survey. Available at: http:// http://www.cdc.gov/nchs/about/major/nhis/released200603.htm. Accessed September 19, 2006.
3. American Diabetes Association. Economic costs of diabetes in the U.S. in 2002. Diabetes Care. 2003;26(3):917–932.
4. American Diabetes Association. Standards of medical care in diabetes–2006. Diabetes Care. 2006;29(supp 1):S4–S42.
5. Harris MI, Eastman RC, Cowie CC, et al. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999;22(3):403–408.
6. Brandt I, Joossens J, Chen X, et al. Inhibition of dipeptidyl-peptidase IV catalyzed peptide truncation by vildagliptin ((2S)-{[(3-hydroxyadamantan-1-yl)amino]acetyl}-pyrrolidine-2-carbonitrile). Biochem Pharmacol. 2005;70:134–143.
7. Duttaroy, Voelker F, Merriam K, Zhang X, et al. The DPP-4 inhibitor vildagliptin increases pancreatic beta cell neogenesis and decreases apoptosis [abstract]. American Diabetes Association 65th Annual Scientific Sessions; June 10–14, 2005; San Diego, Calif. Abstract 572-P.
8. Duttaroy A, Voelker F, Ren X, Zhang X, et al. Head-to-head comparison of the DPP-4 inhibitor vildagliptin with exendin-4 in a model of pancreatic beta cell injury [abstract]. American Diabetes Association 65th Annual Scientific Sessions; June 10–14, 2005; San Diego, Calif. Abstract 267-OR.
9. Villhauer EB, Brinkman JA, Naderi GB, et al. 1-[[(3-hydroxy-1-adman-tyl)amino}acetyl}-2-cyano-(S) pyrrolidine: a potent, selective and orally bioavailable di-peptidyl peptidase IV inhibitor with antihyperglycemia properties. J Med Chem. 2003;46:2774–2789.
10. Ahren B, Landin-Olsson M, Jansson PA, Svensson M, et al. Inhibition of dipeptidyl peptidase-4 reduces glycemia, sustains insulin levels, and reduces glucagon levels in type 2 diabetes. J Clin Endocrinol Metab. 2004;89:2078–2084.
11. He Y, Sabo R, Wang Y, et al. The influence of hepatic impairment on the pharmacokinetics of vildagliptin [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 2024-PO.
12. Balas B, Baig M, Watson C, Dunning BE, et al. Vildagliptin suppresses endogenous glucose production (EGP) and increases beta cell function after single dose administration in type 2 diabetic patients [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 122-OR.
13. Pratley RE, Jauffret-Kamel S, Galbreath E, Holmes D. Twelve-week monotherapy with the DPP-4 inhibitor vildagliptin improves glycemic control in subjects with type 2 diabetes. Horm Metab Res. 2006;38:423–428.
14. Pratley R, Galbreath E. Twelve-week monotherapy with the DPP-4 inhibitor, LAF237 improves glycemic control in patients with type 2 diabetes (T2DM) [abstract]. American Diabetes Association 64th Annual Scientific Sessions; June 4–8, 2004; Orlando, Fla. Abstract 355-OR.
15. Kelley DE, Dunning BE, Ligueros-Saylan M, Holst JJ, et al. Four-week treatment with vildagliptin increases fasting plasma levels of intact incretin hormones both in patients with type 1 (T1DM) and type 2 (T2DM) diabetes [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 1481-P.
16. D'Alessio DA, Watson C, He Y, Ligueros-Saylan M, et al. Restoration of an acute insulin response to glucose in drug-naïve patients with type 2 diabetes (T2DM) by 3-month treatment with vildagliptin [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 454-P.
17. Matikainen N, Manttari S, Schweizer A, Ulvestad A, et al. Vildagliptin therapy reduces postprandial intestinal triglyceride-rich lipoprotein particles in patients with type 2 diabetes. Diabetologia. 2006;49(9):2049-2057.
18. Garber A, Camisasca, RP, Ehrsam E, Collober-Maugeais C, et al. Vildagliptin added to metformin improves glycemic control and may mitigate metformin-induced GI side effects in patients with type 2 diabetes (T2DM) [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 121-OR.
19. DeJager S, Lebeaut A, Couturier A, Schweizer A. Sustained reduction in HbA1c during one-year treatment with vildagliptin in patients with type 2 diabetes (T2DM) [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 120-OR.
20. Ahren B, Gomis R, Standl E, Mills D, Schweizer A. Twelve- and 52-week efficacy of the dipeptidyl peptidase IV inhibitor LAF237 in metformin-treated patients with type 2 diabetes. Diabetes Care. 2004;27:2874–2880.
21. Ahren B, Pacini G, Foley JE, Schweizer A. Improved meal-related beta-cell function and insulin sensitivity by the dipeptidyl peptidase-IV inhibitor vildagliptin in metformin-treated patients with type 2 diabetes over 1 year. Diabetes Care. 2005;28:1936–1940.
22. Rosenstock J, Baron MA, Schweizer A, Mills D, DeJager S. Vildagliptin is as effective as rosiglitazone in lowering HbA1c but without weight gain in drug-naïve patients with type 2 diabetes (T2DM) [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 557-P.
23. Serra DB, He Y, Wang Y, Riviere G, et al. Combination of the DPP-4 inhibitor vildagliptin (LAF237) with pioglitazone is safe and well tolerated with no pharmacokinetic interaction [abstract]. American Diabetes Association 65th Annual Scientific Sessions; June 10–14, 2005; San Diego, Calif. Abstract 2192-PO.
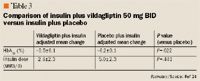
24. Fonseca V, DeJager S, Albrecht D, et al. Vildagliptin as add-on to insulin in patients with type 2 diabetes (T2DM) [abstract]. American Diabetes Association 66th Annual Scientific Sessions; June 6–13, 2006; Washington, DC. Abstract 467-P.
25. Pratley RE, Jauffret-Kamel S, Galbreath E, Holmes D. Twelve-week monotherapy with the DPP-4 inhibitor vildagliptin improves glycemic control in subjects with type 2 diabetes. Horm Metab Res. 2006;38:423–428.
26. Ristic S, Byiers S, Foley J, Holmes D. Improved glycaemic control with dipeptidyl peptidase-4 inhibition in patients with type 2 diabetes: vildagliptin (LAF237) dose response. Diabetes Obesity Metab. 2005;7:692–698.
27. Barilla D, Yanling H, Balez S, et al. No pharmacokinetic interactions or acute clinical safety issues preclude combination of the DPP-4 inhibitor LAF236 with glyburide [abstract]. American Diabetes Association 64th Annual Scientific Sessions; June 4–8, 2004; Orlando, Fla. Abstract 1967-PO.
